GENERAL INFORMATION
• Benign soft tissue tumor arising from a peripheral nerve sheath (epineurium) derived from a schwann cell.
• Also known as Neurilemoma
• Arises from the periphery of the nerve, epineurium
• The nerve is displaced eccentrically
• Small cutaneous nerves may appear to be obliterated by the tumor
• Excision of the tumors sometimes causes nerve damage or compromises the affected nerve.
• Clinically difficult to distinguish Schwannomas from malignant peripheral nerve sheath tumor (MPNST).
CLINICAL DATA
• 5% of benign soft tissue tumors
• Difficult to distinguish Schwannomas from malignant peripheral nerve sheath tumors
• Most schwannomas are less than 5 cm while most MPNST are greater than 5 cm
• Low rate of local recurrence <1%.
• Malignant degeneration is extremely rare.
DIFFERENTIAL DIAGNOSIS
• MPNST
• Neurofibroma
• Cyst of nerve sheath
CLINICAL PRESENTATION
Signs/Symptoms
• Typically a painful mass particularly when pressure applied to mass; Can also be painless
o Sometimes complain of referred pain in the distribution of the involved nerve
• Slowly growing mass
o Usually <5cm
o +Tinel’s sign
o Mobile in transverse plane but no in longitudinal plane
• Occasionally, neurological difficulties may occur
Prevalence
• 5% of benign soft tissue tumors
• No predilection for any particular sex or race
Age:
• Occurs in all ages
• Most commonly found in individuals between 20 and 50 years of age
Sites
• Most commonly found at major peripheral nerves of the head, neck, and flexor surfaces of the upper extremities and extremities
• May involve nerve roots from spine
• Multiple may occur along course of a nerve
Radiographic Presentation
Plain x-ray appearance
• Radiographs usually appear normal
o May reveal nonspecific soft tissue mass
o Mature areas of osteoid or chondroid mineralization may very rarely occur
MRI appearance (Fig. 1 – 4)
• Intermuscular mass closely related to a neurovascular bundle with a distinct margin surrounded by rim of fat (split fat sign)
• Fusiform, elongated cigar shaped mass
• Nerve: Tubular structure visualized entering and exiting the mass (may be difficult to see with small lesions or lesions of the trunk or retroperitoneum) (Fig. 2 & 4)
• Spinal lesions: usually dumbell shaped exiting from and enlarged neural foramina
• T1: Isointense to muscle; Variable enhancement with gado
• T2: High signal (myxoid areas) with some heterogeneity (Fig. 3)
o Target Sign: Low signal central area (cellular/collagenous area; Antoni A) and high signal peripheral area (myxoid area; Antoni B)
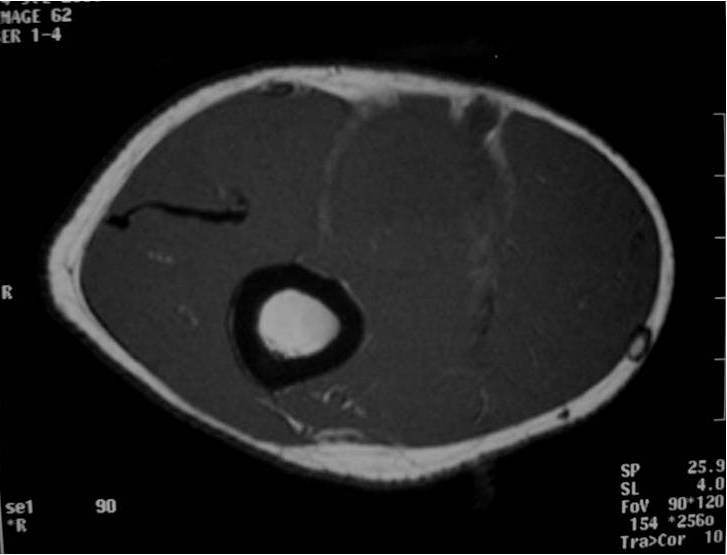

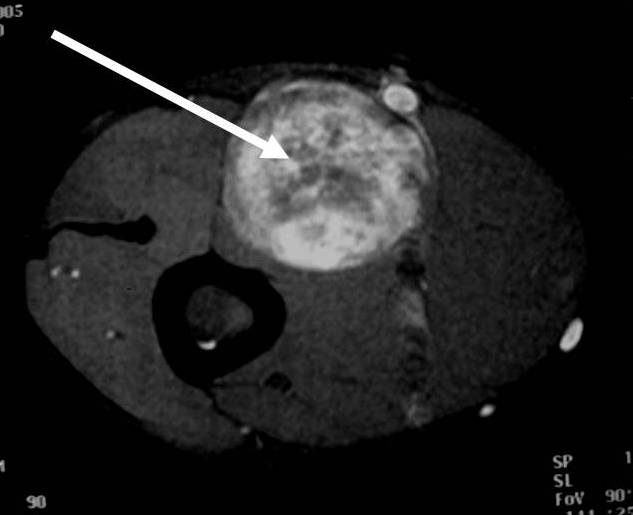
 Fig. 1-4 MR image demonstrates a 5 cm intermuscular mass in the anterior compartment of the arm arising along the course of the neurovascular structures. Isointense to muscle on T1W image and heterogeneous high signal on T2W with low signal in the central area (Antoni A) and peripheral high signal (Antoni B), known as “Target Sign”. Coronal image shows a structure entering and exiting the mass (median nerve).
Fig. 1-4 MR image demonstrates a 5 cm intermuscular mass in the anterior compartment of the arm arising along the course of the neurovascular structures. Isointense to muscle on T1W image and heterogeneous high signal on T2W with low signal in the central area (Antoni A) and peripheral high signal (Antoni B), known as “Target Sign”. Coronal image shows a structure entering and exiting the mass (median nerve).
CT appearance
• Attenuation on noncontrast CT is lower than muscle
Gross Pathology
• Surrounded by capsule of the epineurium
• Tumors surrounding small nerves may eclipse or obliterate the nerve of origin
• Present as eccentric masses, often surrounded by nerve fibers, when they originate from large nerves
• Tumors have a white, or yellow appearance and are usually less than 5 cm in diameter
Microscopic Pathology
• Usually uninodular masses
• Surrounded by fibrous capsules consisting of epineurium and residual nerve fibers
• Distinct Pattern of alternating Antoni A and B areas
o Antoni A Area: Cellular area arranged in short bundles or interlacing fascicles
Spindle cells with wavy appearing nuclei. (Fig. 5 & 6)
o Antoni B Area: Less cellular and more myxoid (Fig. 7)
• Ancient schwannomas: a type of schwannoma that is typically larger and demonstrates cyst formation, calcification, hemorrhage, fibrosis. Ancient schwannomas can be mistaken for malignant peripheral nerve sheath tumors
• Mitotic activity is rare.
• S-100 positive staining; Vimentin positive
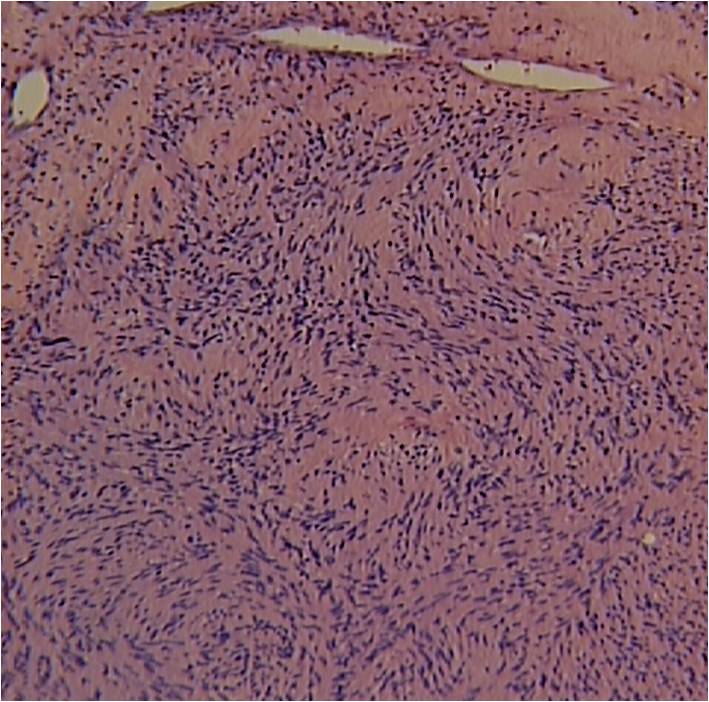
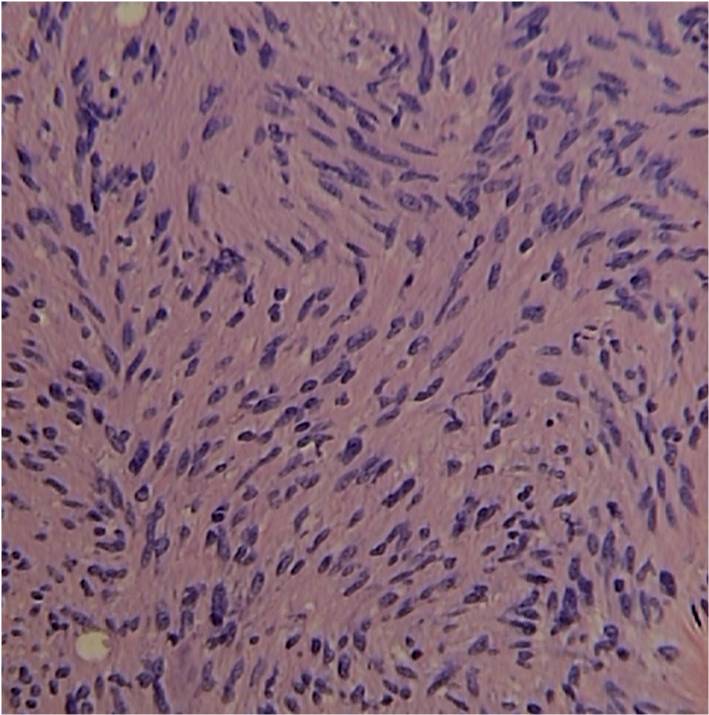
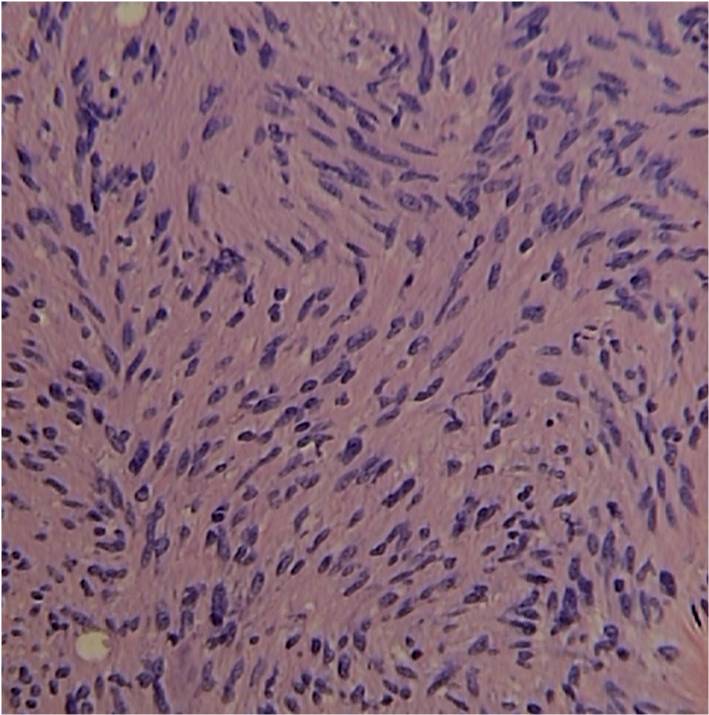 Fig. 5-7 Microscopic Pathology demonstrates 2 different patterns; Antoni A area with spindled hypercellular distribution with wavy appearing nuclei (Fig 5 & 6A) that palisades, known as Verocay Bodies (Fig 6B). Antoni B area is less cellular and more myxoid (Fig 7) than the Antoni A area. Mitotic activity is not visible.
Fig. 5-7 Microscopic Pathology demonstrates 2 different patterns; Antoni A area with spindled hypercellular distribution with wavy appearing nuclei (Fig 5 & 6A) that palisades, known as Verocay Bodies (Fig 6B). Antoni B area is less cellular and more myxoid (Fig 7) than the Antoni A area. Mitotic activity is not visible.
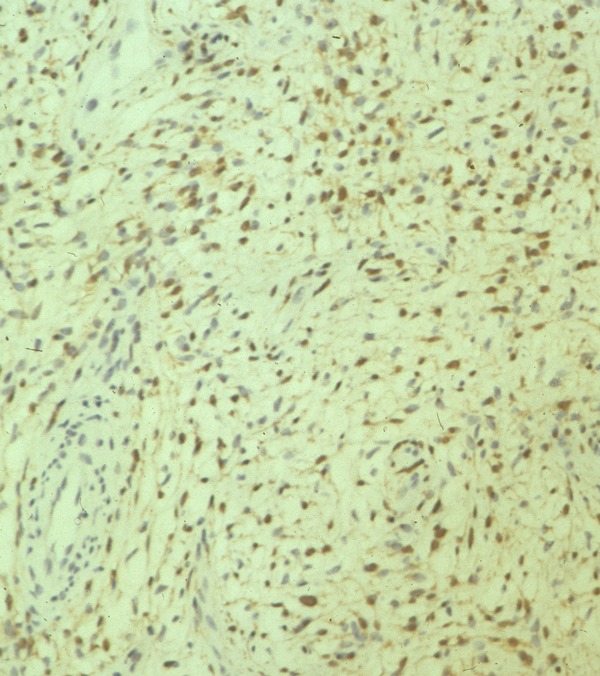 Fig. 8 Inmunohistochemistry. Schwannoma has a strong positive S-100 staining.
Fig. 8 Inmunohistochemistry. Schwannoma has a strong positive S-100 staining.
Treatment
• Surgical Excision (Fig. 9, 10, 11)
o Marginal Excision; Spare nerve from excision
The epineurium is opened carefully on a side opposite nerve fascicles and the mass is gently separated from the nerve fascicles and epineurium.
o Rarely if ever recurs
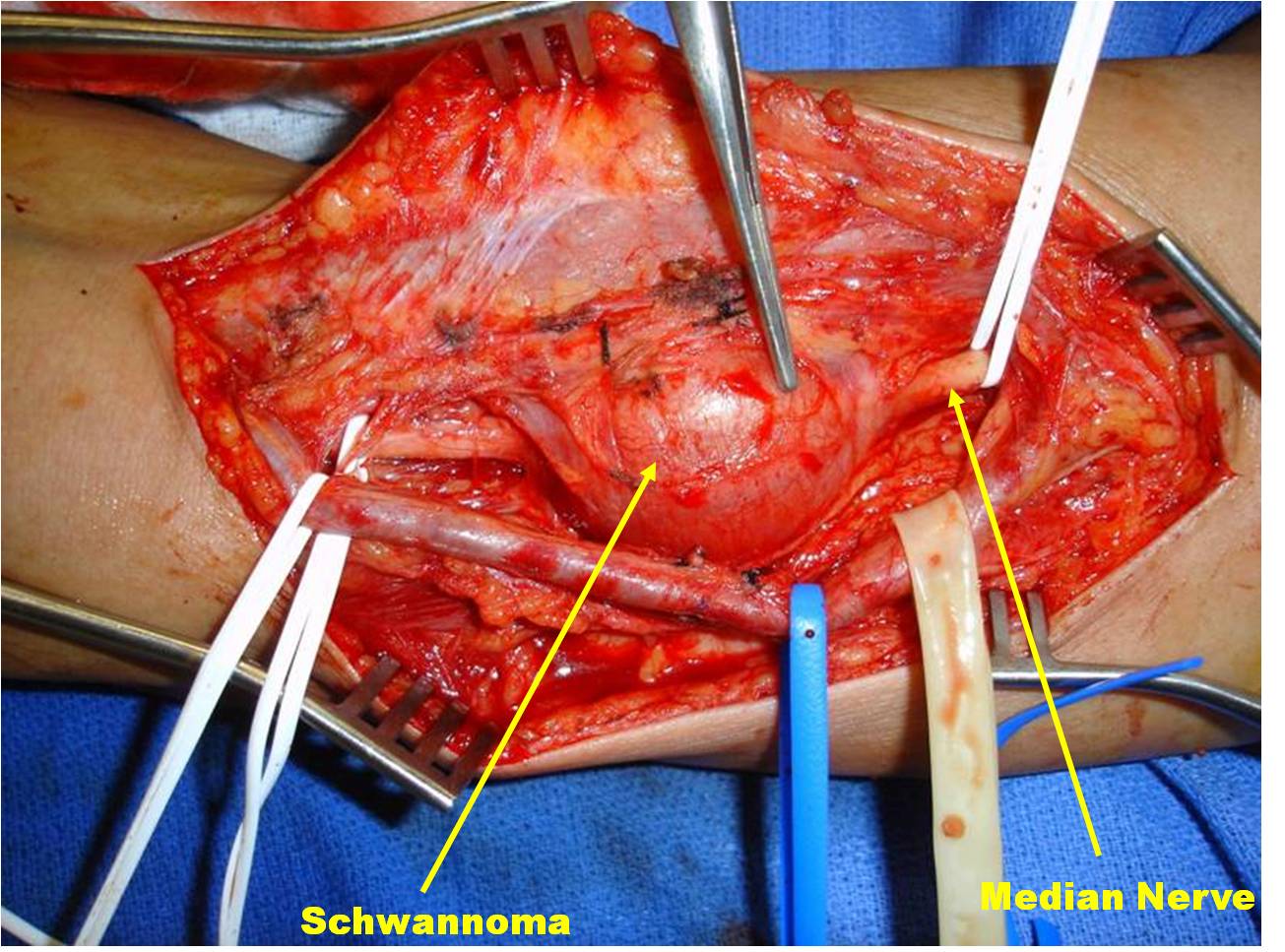
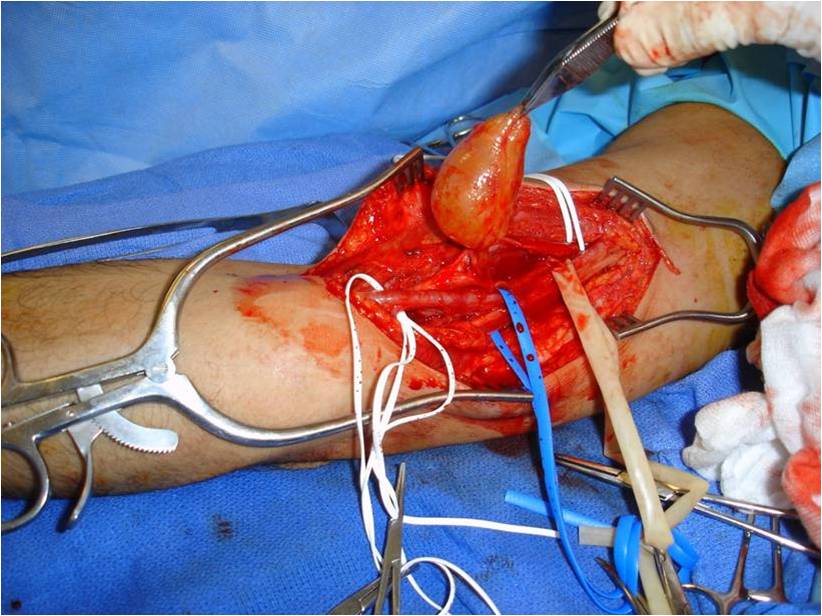
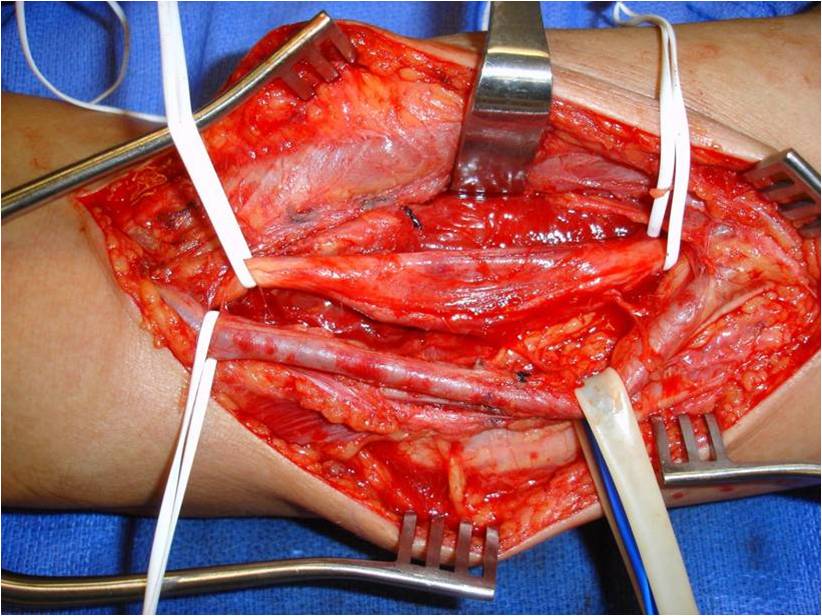 Fig. 9-11 Intraoperative photographs demonstrate medial approach to the arm and neurovascular dissection, including; median nerve and brachial artery. Schwannoma is easily distinguished in the median nerve. The sheath of the nerve is opened on the opposite side of the splayed out nerve fascicles and the tumor removed. The nerve was spared.
Fig. 9-11 Intraoperative photographs demonstrate medial approach to the arm and neurovascular dissection, including; median nerve and brachial artery. Schwannoma is easily distinguished in the median nerve. The sheath of the nerve is opened on the opposite side of the splayed out nerve fascicles and the tumor removed. The nerve was spared.
Prognosis / Biological Behavior
• Consists almost exclusively of Schwann cells
• Strong expression of S-100 protein
• Multiple neurilemomas will rarely occur
o Neurofibromatosis 1 associated with multiple schwannomas
• Benign tumor, does not metastasize
• Local recurrence rare <1%
• Pain usually relieved with removal
• Malignant degeneration is exceedingly rare.
