General Information
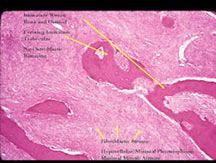
- Parosteal osteosarcoma is a low grade, well differentiated fibroblastic tumor that produces bone/osteoid (immature woven bone). It arises from the surface of the bone, namely the outer layer of the periosteum. It is slow growing and slow to metastasize.
- Most common type of juxtacortical/surface osteosarcoma
- Represents approximately 5% of all types of osteosarcomas
- Derived from the outer layer of periosteum and therefore does not elevate the periosteum as it grows. Radiographically, there is no associated periosteal reaction
- Usually a low grade tumor with fibroblastic stroma and osteoid/woven bone
- Low risk of metastasizing or spreading: approximately 10%-15% risk of metastasis when presents early (when entire tumor is low grade)
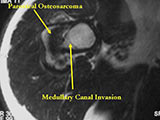
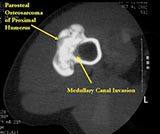
- Parosteal osteosarcomas that are present for prolonged periods of time may either have areas that become higher grade or dedifferentiate. Dedifferentiation refers to a portion of the tumor changing and becoming a high grade type of sarcoma. In addition, parosteal osteosarcomas that are present for a prolonged period of time can invade the bone (medullary canal) that it arose from. Tumors that have undergone dedifferentiation or invaded the underlying bone are more aggressive and have a higher risk of metastasizing (spreading). This is important to know for treatment purposes. Typically, low grade parosteal osteosarcomas are treated with surgery alone. Parosteal osteosarcomas with high grade areas may also be treated with chemotherapy in addition to surgery.
Clinical Presentation
Signs/Symptoms: Painless slowly enlarging firm immobile mass in an extremity (most commonly posterior distal thigh/popliteal fossa behind the knee)
- Mass may be present for several years (usually for more than a year and some patients have reported symptoms for more than a decade)
Prevalence: Female>Male 2:1
Age: 20-40 yrs
- Usually occurs about a decade older than conventional osteosarcoma
- Peak age is in the 20s
- Has been reported in patients in their 6th or 7th decades of life.
Sites:
- Posterior distal femur metaphysis (65%)
- Presents as a mass in popliteal fossa
- Proximal humerus (15%); Tibia (10%); Fibula (3%), Radius, Ulna
Radiology
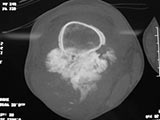
X-Rays:
- Lobulated and ossified exophytic mass (cauliflower-like) adjacent to the cortex; attached to metaphyseal cortex via a broad base
- Centrally, the tumor is radiodense (demonstrates ossification)
- Peripherally there may be small radiolucies that represent low grade cartilaginous lobules, fibrous tissue or fat
- The underlying cortex may be thickened
- There is no periosteal reaction since the tumor comes from the outer layer of the periosteum and therefore does not elevate the periosteum.
- Large tumors encircle the bone
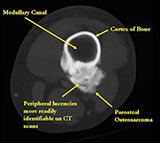
- Appears to have broad attachment to underlying cortex with a cleft between exophytic base and cortex at periphery. This is referred to as a "String Sign" (cleft is often only identifiable on CT scan)
- There may be invasion of the medullary canal with long standing disease
- High grade or defifferentiated areas may appear as large radiolucent areas/mass adjacent to radiodense areas
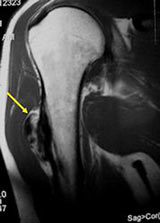
MRI/CT:
- Useful for determining medullary invasion
- Can help discern areas that may be high grade
- Most useful for evaluating the local extent of the tumor and relationship to neurovascular structures the circumference of the femur involved by the tumor (important for surgical planning)
- CT of chest is used for detecting pulmonary metastases
| Roll over the images for more information |

Click here for larger image |

|

|
|
 
|

|
|
|
|

|
|
|
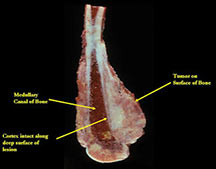
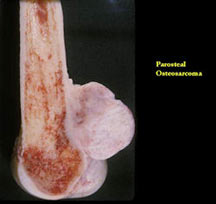
Pathology
- Firm, exophytic bony mass fixed to cortex by means of a broad base
- If it has grown through the cortex, there may be an intramedullary component
- There may be a cartilaginous cap similar to an osteochondroma
- Grows along long axis of bone and around the circumference of the bone
- Satellite nodules may be present, especially with recurrent tumors
- Tan to ivory in color
| Roll over the images for more information |
|
|
Microscopic Pathology
| Roll over the images for more information |
|
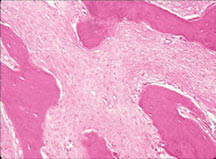
|
Treatment/Surgery
| Roll over the images for more information |

|

|
Prognosis
- There is an 80-90% cure rate for low grade parosteal osteosarcomas treated with surgery alone
- Metastases more common with medullary invasion, high grade components (grade 3) and dedifferentiation (grade 3 tumors)
- Intermediate grade (grade 2) tumors have a worse prognosis than the more typical grade 1 (low grade tumors)
- Many parosteal osteosarcomas with intramedullary extension are higher grade lesions or dedifferentiated tumors
- If present for prolonged periods before being identified, may dedifferentiate & develop high-grade areas
- Higher grade variants have a higher likelihood of spreading
- May be treated with chemotherapy in addition to surgery
