General Information
- Osteochondroma is an outgrowth of medullary and cortical bone
- A portion of the cartilaginous growth plate grows outward instead of longitudinally and forms the osteochondroma/exostosis (like a branch on a tree)
- It consists of bone covered with cartilaginous cap (exostosis)
- May be secondary to a growth plate injury (Node of Ranvier injured)
- Osteochondromas are benign, non-neoplastic conditions
- Hamartomatous anomaly
- It can occur as a solitary lesion or as multiple exostoses associated with a hereditary condition known as Multiple Hereditary Exostoses (MHE)
- Radiation exposure can also be a cause of multiple osteochondromas
- Solitary Osteochondromas are the most common benign bone tumors and constitute 35% of all benign bone tumors and 10% of all bone tumors overall
There are 2 forms
- Pedunculated (with a stalk)
- Sessile (flat without a stalk)
- Osteochondromas likely arise from displaced cartilage through periosteal defect and grow at right angles to normal growth plate
- Lesions have self-limited growth that ceases after skeletal maturity
- Due to endochondral ossification, cartilage cap diminishes in thickness as age increases
Osteochondroma -(most common benign neoplasm of bone that leads to biopsy)
Types:
- Solitary Osetocartilaginous Exostosis
- Hereditary Multiple Exostoses (HME)
Radiographic Subtypes:
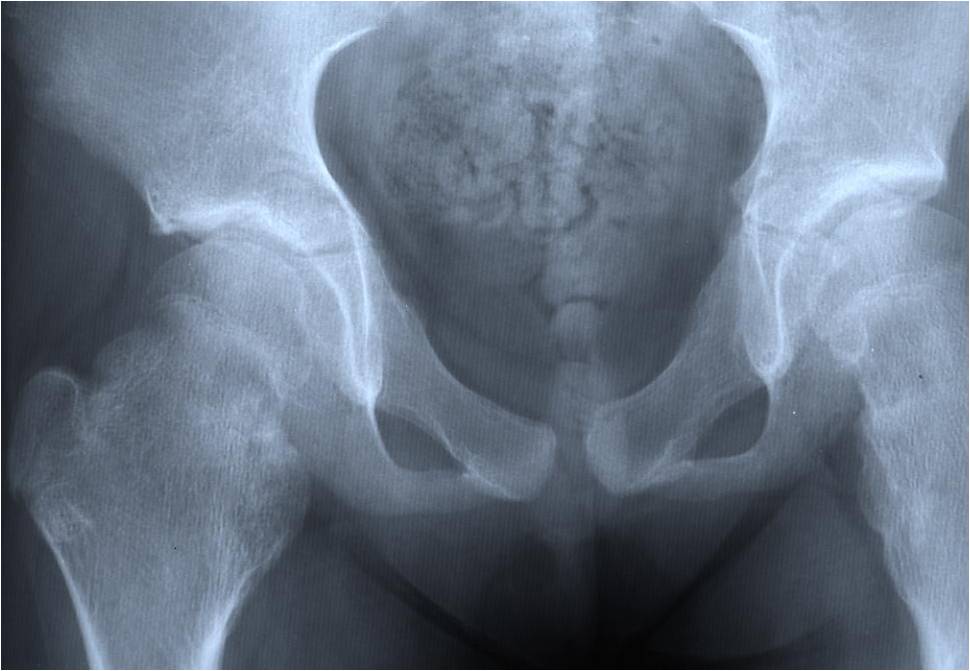
Multiple Heredity Exostoses (MHE)
Clinical Data:
- Male predominance (3:1)
- Autosomal Dominant inheritance
- There is variability in size and number of ostechondromas (variable penetrance)
- Any portion of the skeleton preformed in cartilage may be involved
- Evident during childhood
- MHE may be bilaterally symmetric
- One side may predominate
- There is a higher incidence of malignant transformation (10-20%) of osteochondromas that
- develop in MHE. Most commonly a secondary low grade chondrosarcoma develops.
Clinical Presentation
Signs/Symptoms:
- Hard swelling for many years
- Symptoms dependent on location/size
- May cause mechanical symptoms from compression of adjacent structures such as tendons,
- nerve or blood vessels
- An overlying bursa may form and result in a bursitis
- Rare vascular injuries and arterial aneurysms from adjacent osteochondromas
- Malignant Transformation: Solitary osteochondroma <1%
- Prevalence:
- Male>Female 1.8:1
Age:
- Usually presents clinically by the third decade of life
Sites:
- Appendicular skeleton: Femur (30%) Tibia (20%) Humerus (2-%) Hand and Foot (10%)
- Pelvis (5%) Scapula (4%)
- Surface of metaphyseal portions of long tubular bones
- Knee area 35% of cases
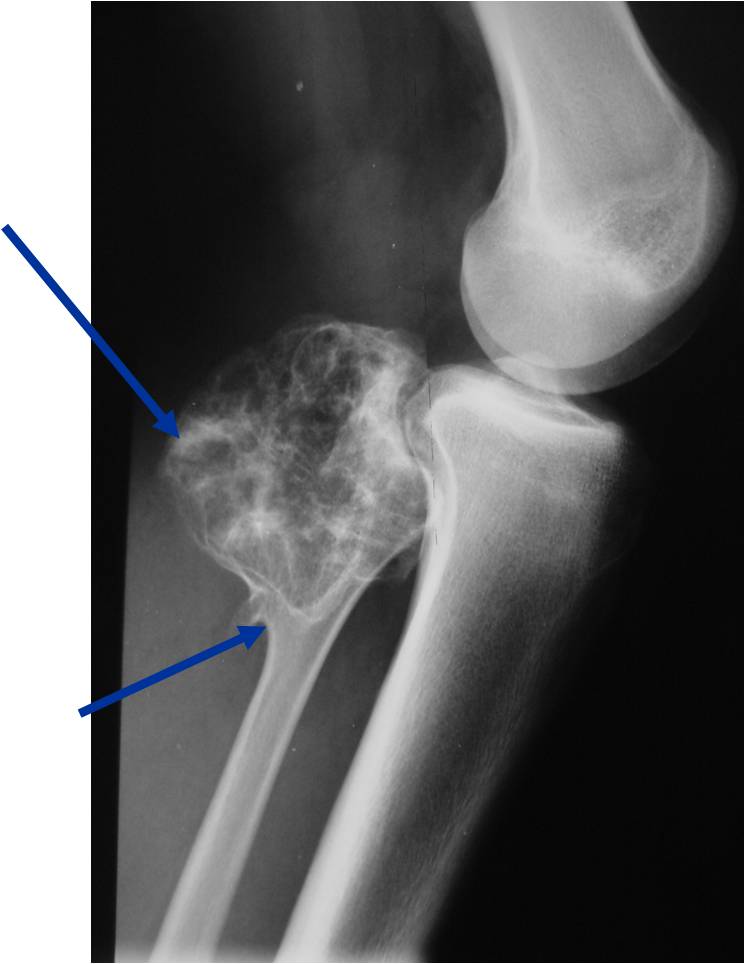
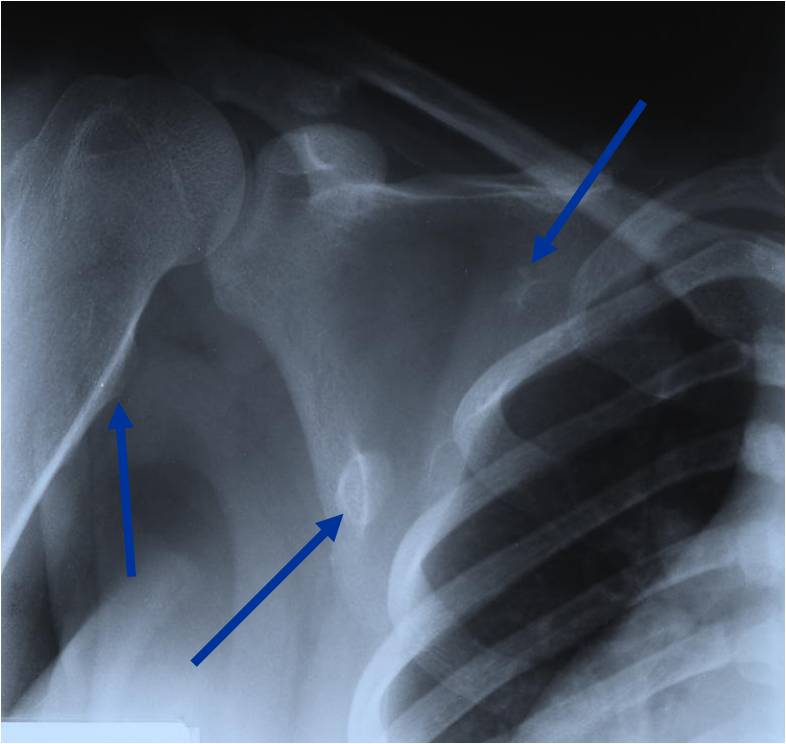
Radiographic Presentation
Plain X-rays:
- Projects from bone with narrow (pedunculated) to broad (sessile) stalk
- Corticomedullary continuity: Medullary bone continuous with that of osteochondroma and cortex blends with that of osteochondroma
- Calcification in cartilaginous cap ("Ring and Arc" and stippled calcifications)
- Lobular growth pattern
- Long bones: arise from metaphysis, grows away from epiphysis toward diaphysis,
- May be associated with failure of tubulation in Multiple Hereditary Exostosis
- Flat bones: tend to be larger and sessile, variable appearance
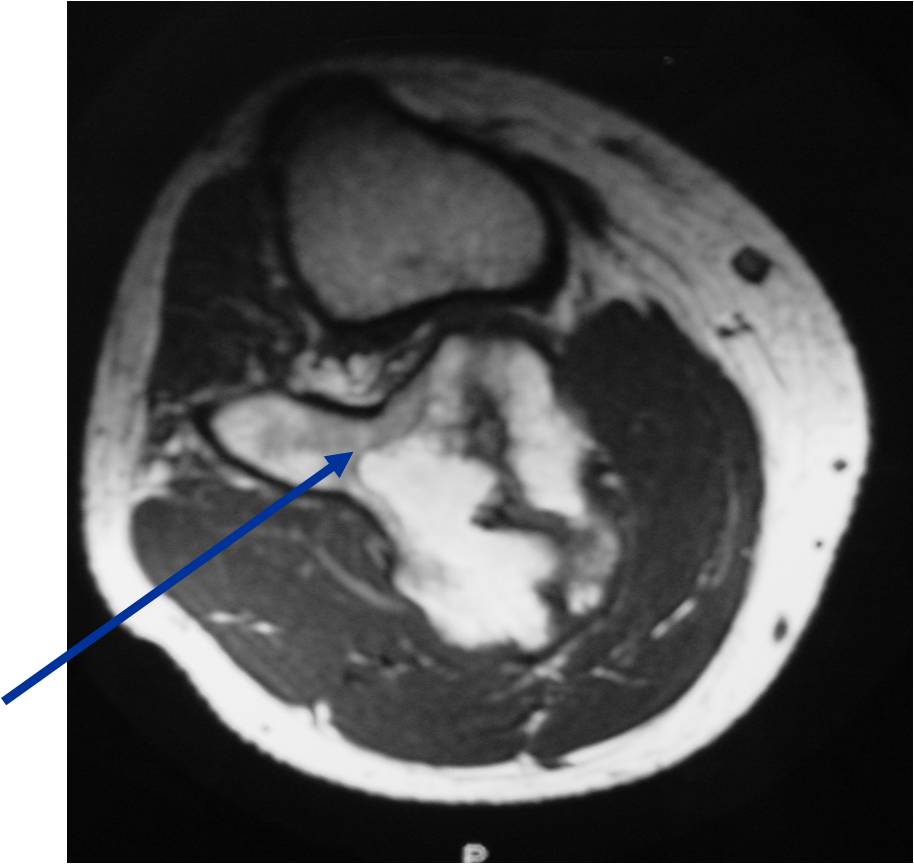
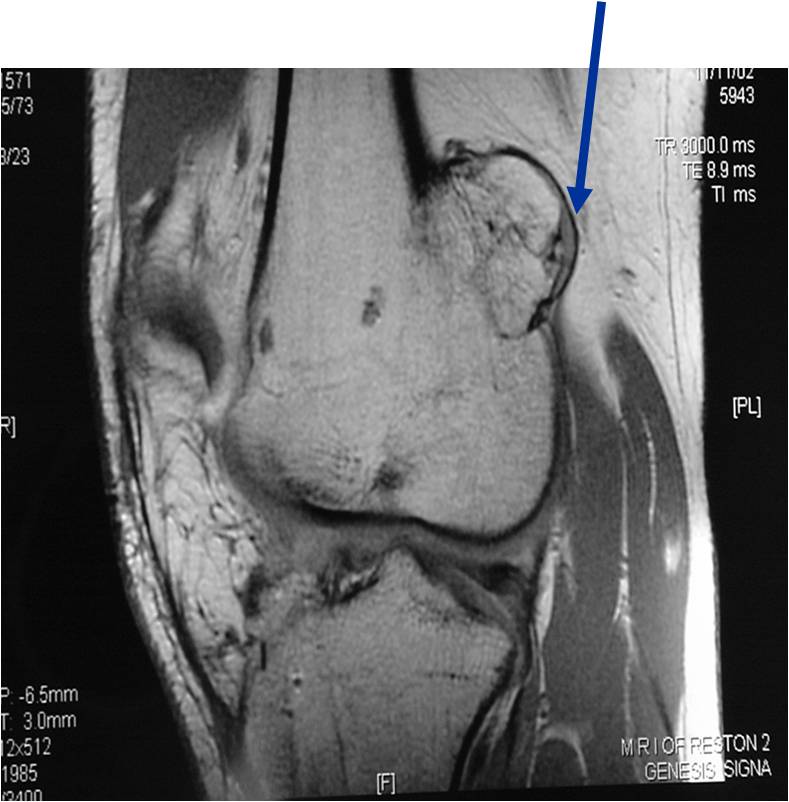
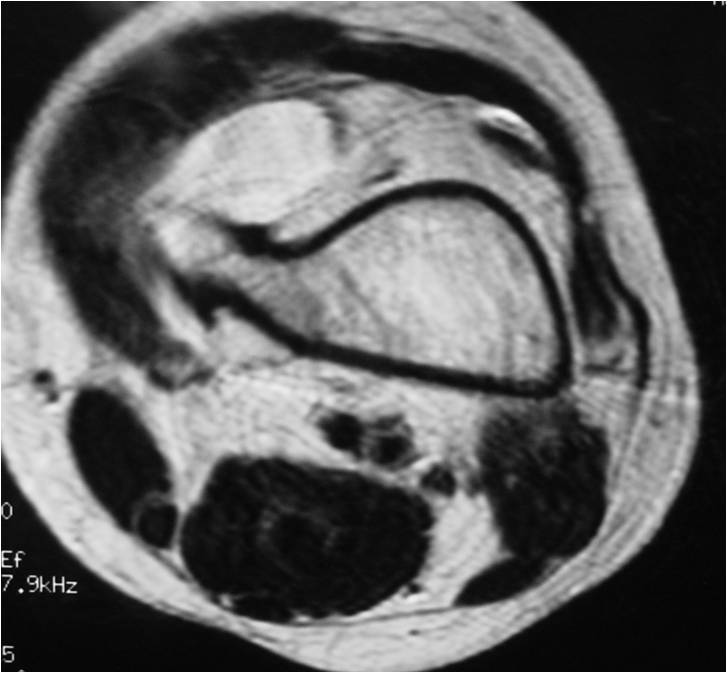
- Cartilage cap thickness is visualized best on MRI, not XR
- Bursa may exist external to cartilage cap (seen on MRI)
| Roll over the images for more information |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
 |
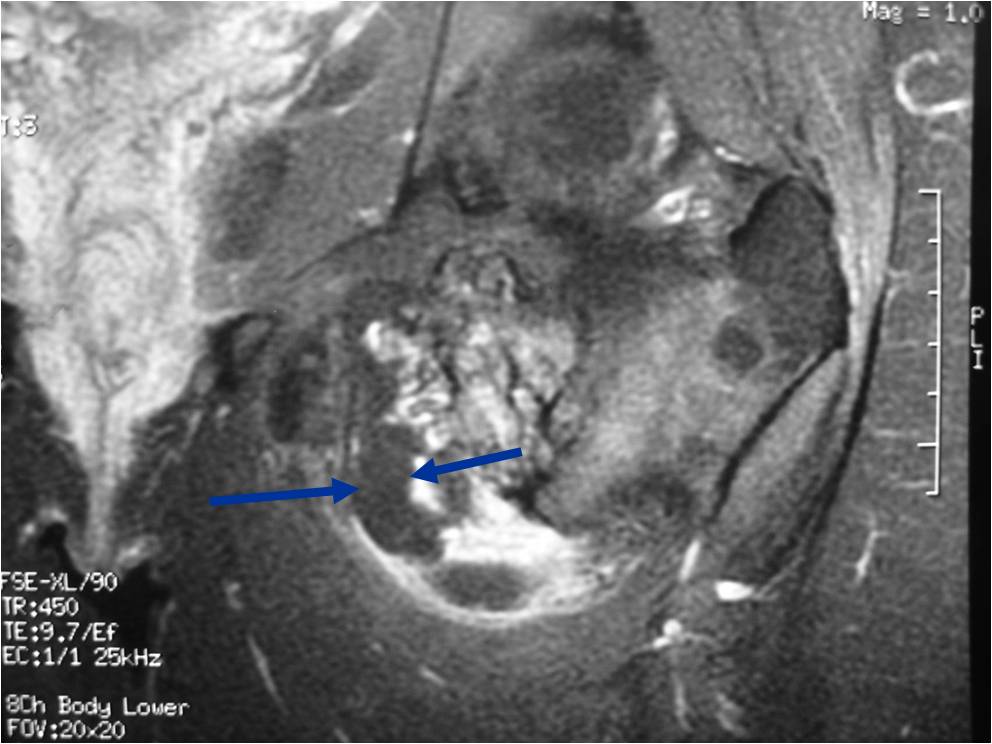
Osteochondroma Vs. Secondary Chondrosarcoma
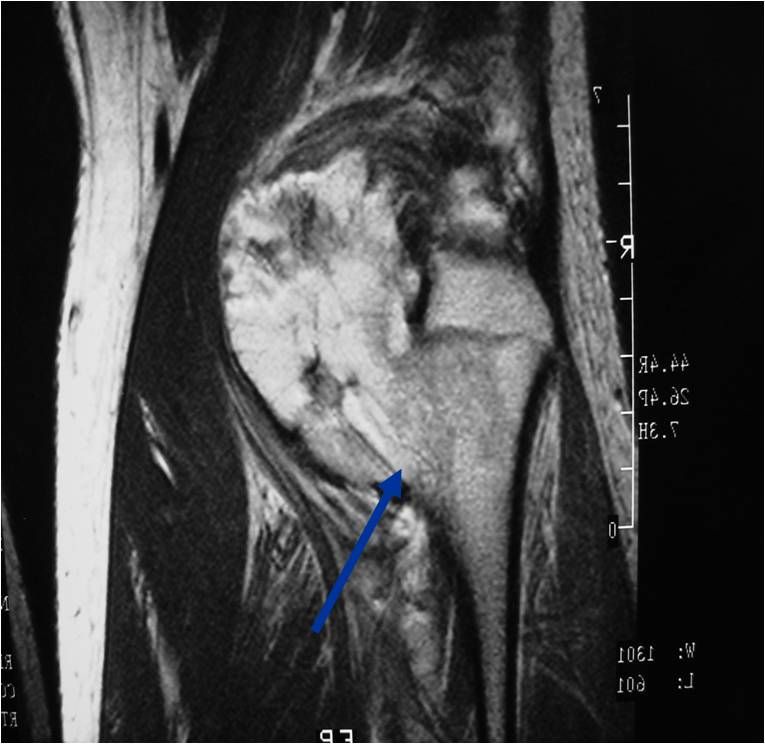
The cartilaginous cap deserves the most attention when differentiating a benign osteochondroma from a secondary chondrosarcoma that arose from a pre-existing osteochondroma
In adults, the cartilaginous cap regresses and becomes thin due to enchondral ossificastion of the majority of the cap.
Malignant transformation is suggested by:
- Cartilaginous cap thickness greater than 2cm
- Cortical destruction
- Backgrowth of the cartilaginous cap into the stalk or medullary canal
- Lysis of calcifications in cap
Osteochondroma: Cartilage Cap
Radiographs
- Chondroid Calcification in cap
- Increasing destruction or change in appearance is worrisome for malignancy
Ultrasound
Bone Scan
- Increased uptake in the cap
MRI:
- Best test for evaluating thickness of cap and surrounding bursa
- Intermediate T1W Images
- High Intensity T2W Images because of fluid content
CT
- The cap will appear as soft tissue with calcification
- Can be difficult to distinguish from muscle
Cap thickness
- Benign < 1.5cm (0.1 - 3.0cm; Avg. 0.6 - 0.9 cm)
- Malignant > 1.5 cm (1.5 - 12cm; Ave. 6cm)
| Roll over the images for more information |
 |
 |
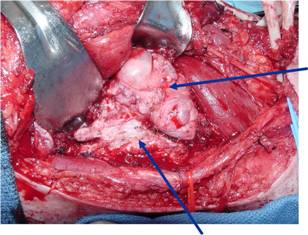
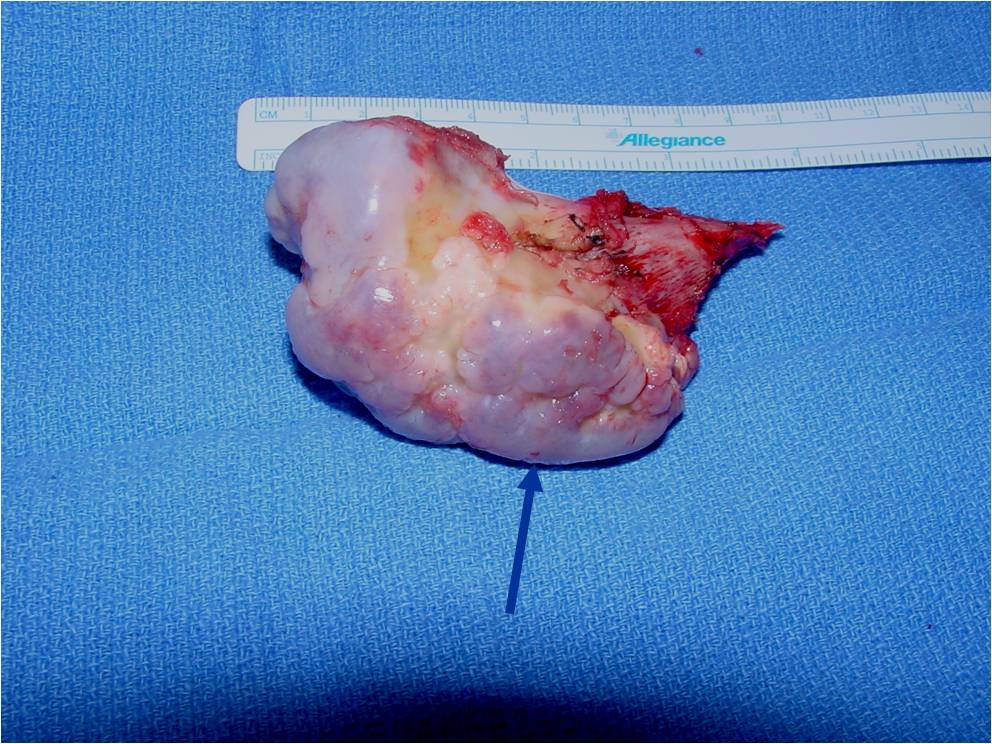
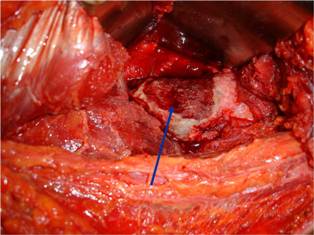
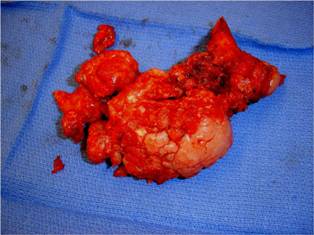
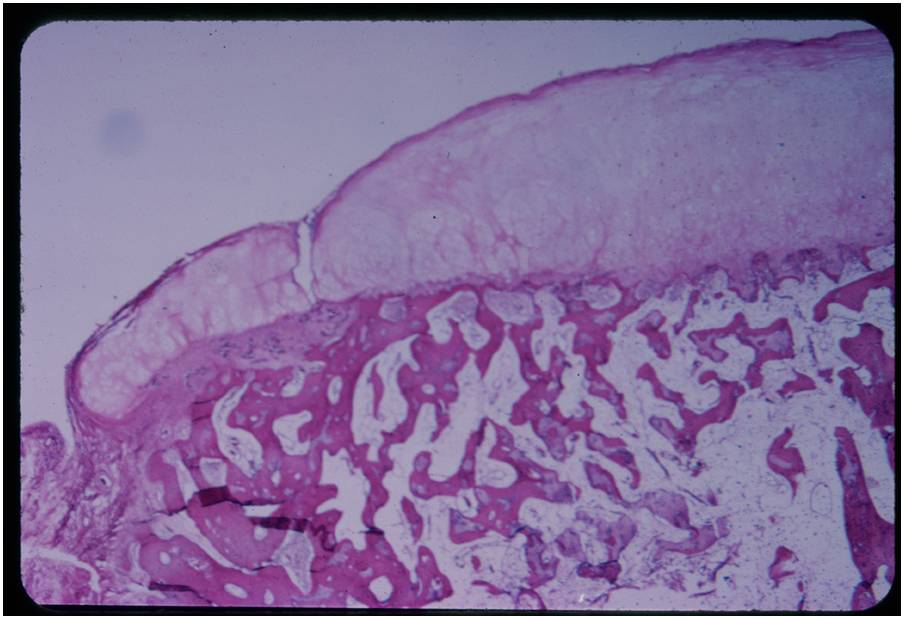
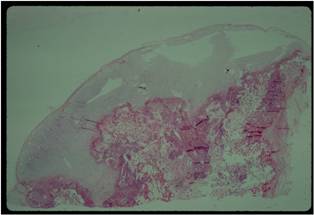
Pathology
Pathology:
- Medullary and cortical continuity w/ underlying bone
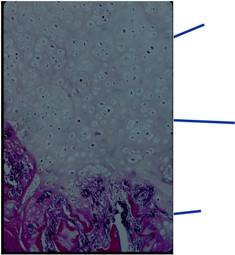
- Hyaline Cartilage Cap with lobular growth
- Cartilage cap involutes after growth
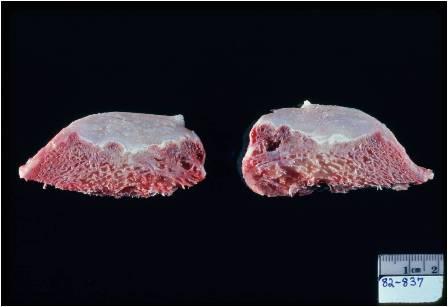
Gross Pathology
- The osteochondroma is completely covered in periosteum
- Cut surface shows hyaline composition of cartilage cap
Cap
- Younger patients thicker cap because of growth hormone
- Smooth or knobby
- 2 mm to 1 cm thick
Beneath the cap, calcified cartilage which appear as white deposits are present
| Roll over the images for more information |
 |
 |
 |
 |
Microscopic Pathology
| Roll over the images for more information |
 |
 |
 |
Treatment
Simple excision:
- Cosmetic reasons
- Impingement on tendons, nerves or blood vessels
- Pain and limitation of motion
- For multiple exostoses, corrective surgery may be necessary due to secondary deformities
Prognosis
- Recurrence after excision is rare
- Rarely, osteochondromas may give rise to malignant chondrosarcoma
- Solitary osteochondromas 1%-2%
- Multiple osteochondromas 5%-25%
- Most common sites to undergo malignant change
- Scapula, pelvis, ribs, proximal femur
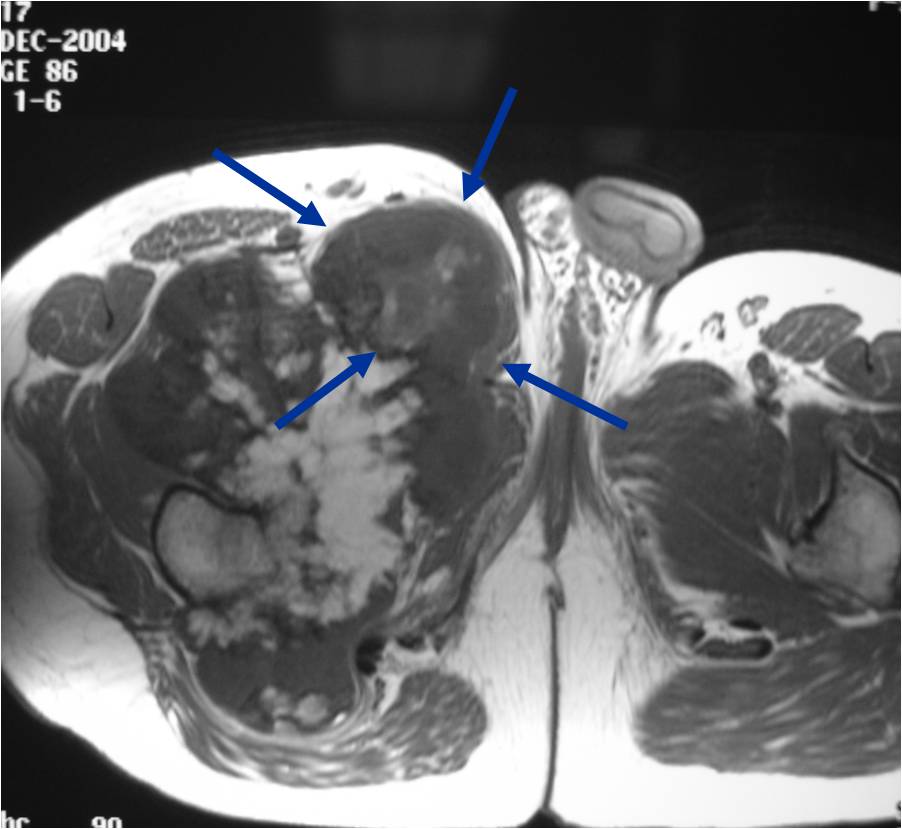
Multiple Heredity Exostoses (MHE)
Clinical Data:
- Male predominance (3:1)
- AD inheritance
- Variability in size and number
- Any portion of the skeleton preformed in cartilage may be involved
- Present in childhood
- May be bilaterally symmetric
- One side may predominate
- Increased incidence of malignant transformation (10-20%)
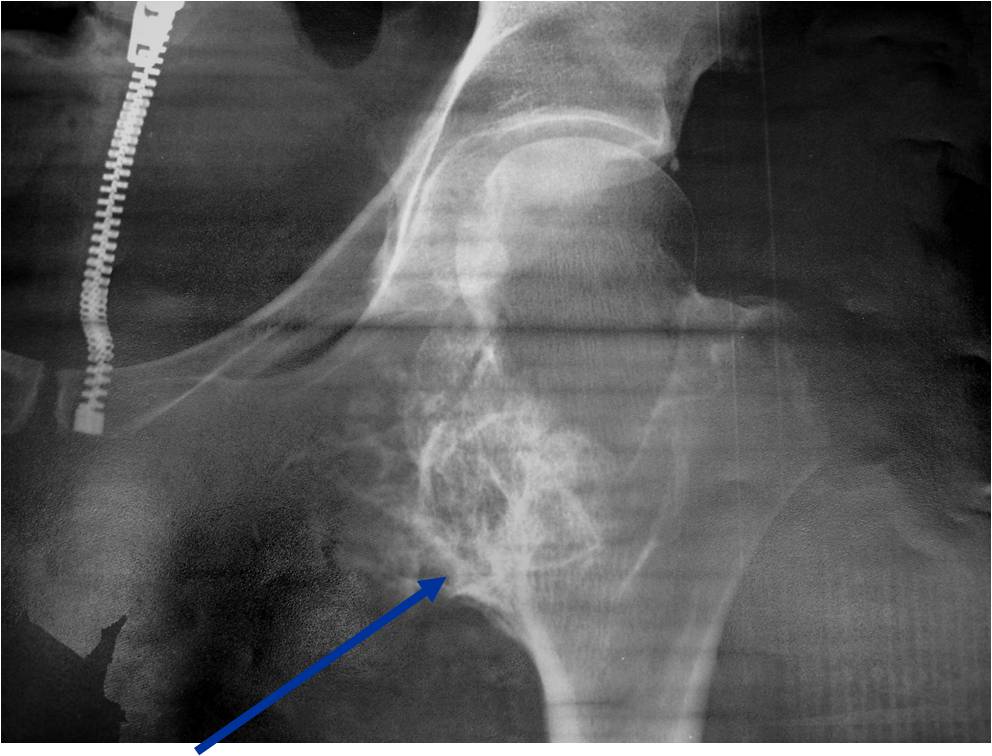
- Radiographically characterized by multiple osteochondromas and undertubulation of bones
- (Erlenmeyer Flask Deformity)
| Roll over the images for more information |
 |
 |
 |
 |
 |
|
Subungal Exostosis - Dupuytren Exostosis
- Osteochondroma Variant
- Females > Males (2:1)
- Often painful and associated with trauma and infection
- Fibrocartilage cap
- Located away from physis
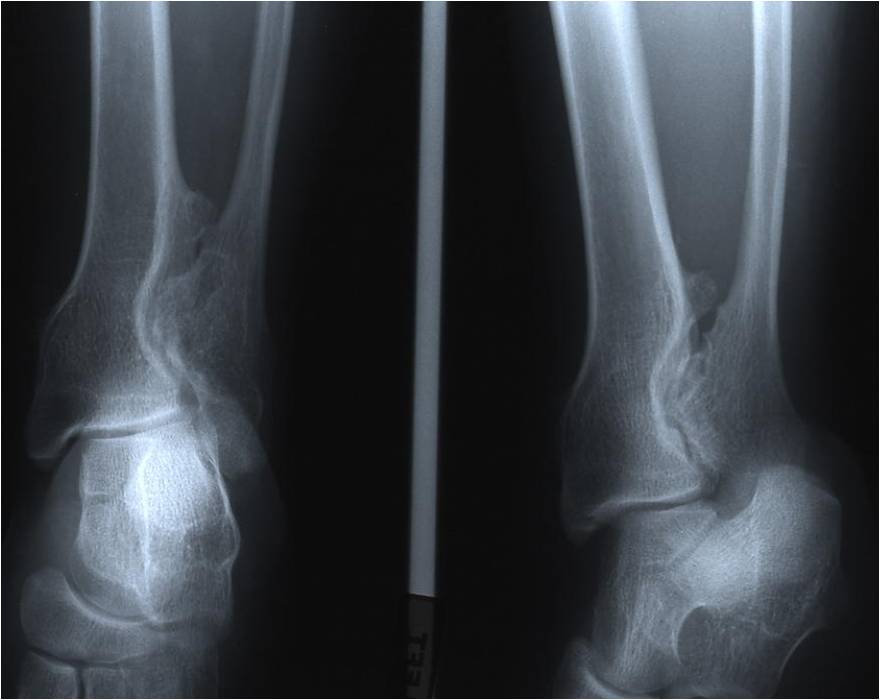
Dysplasia Episphysealis Hemimelica - Trevor Disease
- Male predominance (3:1)
- Very rare < 100 cases
- Swelling, pain and deformity
- Usually lower extremity, unilateral
- 65% multiple done involvement: talus, distal femur, tibia
Dysplasia Episphysealis Hemimelica - Trevor Disease
- Ankle and knee most common
- Medial joint 2X lateral
- Lobular epiphyseal mass
- Histologically identical to an osteochondroma
- May produce deformity and secondary osteoarthritis
