GENERAL INFORMATION
Fibrous dysplasia is not considered a tumor; it is a developmental disorder of the bone. It appears similar to a tumor on radiological studies. Fibrous dysplasia is caused by the inability of the bone-forming tissue to produce mature bone due to a genetic mutation in a G protein. The tissue is arrested at the immature bone stage that consists of fibrous tissue admixed with spicules and islands of woven bone. It can present as a simple isolated bone lesion (monostotic) or as multiple bone lesions (polyostotic). It affects children and adolescents. Patients with the polyostotic form usually have irregular cutaneous cafe-au-lait lesions (skin pigmentation) and an endocrine abnormality, often precocious puberty. Most isolated cases are found incidentally. Some patients particularly those severely affected with the polyostotic form may present with symptoms of swelling, deformity and pain (microfractures). Frank pathologic fracture may occur in some patients. Fibrous dysplasia has a very low risk of malignant transformation. May develop cysts or cartilaginous components and hence termed fibrocystic dysplasia and fibrocartilaginous dysplasia. It may also be the source of an aneurysmal bone cyst.
CLINICAL DATA
• Represent almost 7% of the benign bone abnormalities (tumors)
• > 50% of the cases diagnosed in the first 3 decades of life
• Most patients are asymptomatic and lesion found incidentally
• Slight preference for males
• If the bone growth is involved, may cause deformity such as a shephards crook deformity of the proximal femur
Differential diagnosis
Benign lesion
• Unicameral bone cyst
• Chondromyxoid fibroma
• Aneurysmal bone cyst
• Paget’s disease
• Osteofibrous dysplasia
• Desmoplastic fibroma
• Giant cell reparative granuloma
Malignant lesions
• Osteosarcoma
• Parosteal osteosarcoma
CLINICAL PRESENTATION
Signs/Symptoms
• Pain may be present if bone is weak or fractured
• Localized swelling.
• Cutaneous pigmentation (Café-au-lait spots) may be seen, and is associated with polyostotic disease (Albright’s syndrome).
• Precocious puberty in female patients may be associated with the polyostotic form (McCune-Albright’s syndrome)
• May be associated with soft tissue myxomas (Mazabraud’s syndrome)
Prevalence
• Slight preference for Male>Female (1-1.3:1)
• Age group is between 5 to 20 years
• Peak age second and third decade of life for monostotic form (close to 75%), and polyostotic form usually presents before age of 10 years
Sites
Monostotic
• 80% of cases are:
• Craniofacial bones (30%)
• Femur and tibia (30%)
• Ribs (20%)
Polyostotic
• Between 75% and 90% lesion are located in femur, tibia and pelvis (fig 10-12).
• Remainder is distributed in ribs and skull, but small bones are involved too, like feet bones
RADIOGRAPHIC PRESENTATION
Plain x-ray
• Lesions are metaphyseal and diaphyseal (Fig. 1)
• Preference for the medullary canal
• Lytic lesion, with a “ground glass” appearance; trabeculae appear smudged as though somebody took a pencil eraser and smudged them
• Affected bone may present with a well defined sclerotic, expanded and thick reactive bone called rind of sclerosis
• Pathologic fracture and bowing of the femoral neck (“Shepherd’s crook” deformity) particularly in polyostotic form
CT
• Useful to determine the extent of the lesion as well as ground glass appearance (Fig. 2-3)
• Well defined borders
• Possible endosteal scalloping lesion
• Areas of mineralization within.
MRI
•
MRI can have a very variable appearance and enhancement pattern; May not follow same signal as fibrous tissue which is normally Low signal on T1 and T2
• Low-intermediate heterogenous signal on T1 (Fig. 4)
• Variable heterogeneous signal on T2 (Fig. 5)
• Advantage over other imaging modalities
• Better to evaluate bony lesion extent
• Evaluate cystic degeneration and large lesions
• Useful to assess suspected malignant transformation.
Whole body bone scan
• Increased tracer uptake
• Useful for identify multiple lesions---->polyostotic form
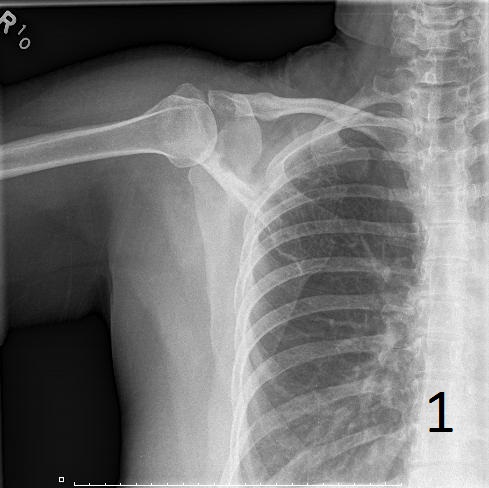
Fig. 1. AP plain x-ray of fibrous dysplasia of the right shoulder showing an expanded lytic lesion involving the spine of the scapula.
.jpg)
Fig. 2. Axial CT reconstruction of the shoulder illustrates a lytic lesion of the right scapula consistent with fibrous dysplasia. There is a ground glass appearance.
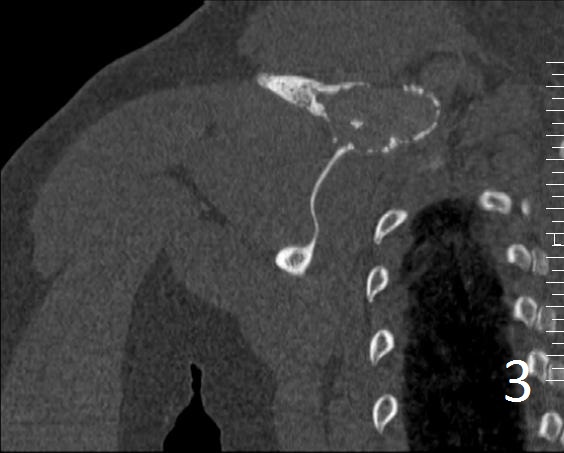
Fig. 3. Coronal CT of the right shoulder shows a expansile lytic lesion with cortical bone expansion.

Fig. 4. Axial T1W of fibrous dysplasia of the scapula shows a lesion with similar signal intensity as muscle.

Fig. 5. Same lesion on Axial T2W FS shows heterogenous signal.
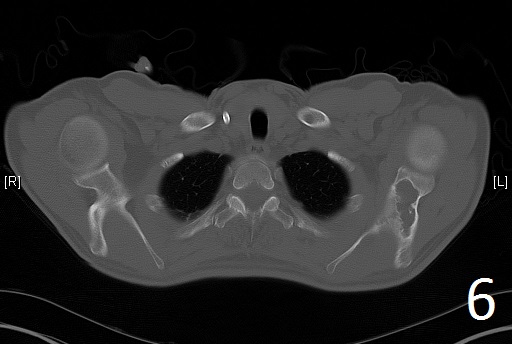
Fig. 6
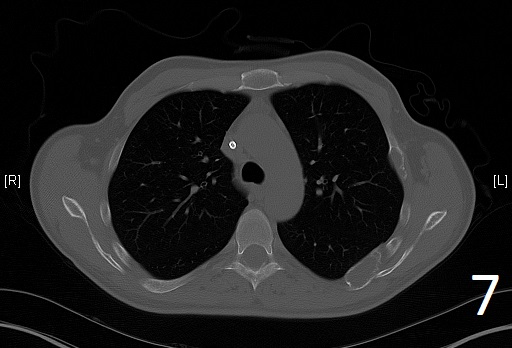
Fig. 7
Fig. 6-7. Axial CT reconstruction of the chest showing lytic and expansile lesion of the left scapula and ribs (polyostotic fibrous dysplasia).
PATHOLOGY
Gross
•
Dense and fibrous tan-gritty tissue
• Cystic formation may be present, filled with clear yellowish fluid but hemorrhagic.
• Dense ossification may also be present.
Microscopic
•
Combination of bland hypocellular fibrous tissue with small fragments of woven bone without visible rimming by osteoblasts(Fig. 7-8) .
• The trabecule are common referred as Chinese characters, or resembling “Cs”and “Os”. Also may be called Alphabet Soup. This arrangement may mimic the appearance of Paget’s diseases
• Trabeculae are not lined with oteoblasts.
• Metaplastic chondroid component could be associated, but not common to be related with cartilaginous neoplasm
• Cystic degeneration, showing high number of lipophages and benign multinucleated giant cells
• No cytologic atypia is seen
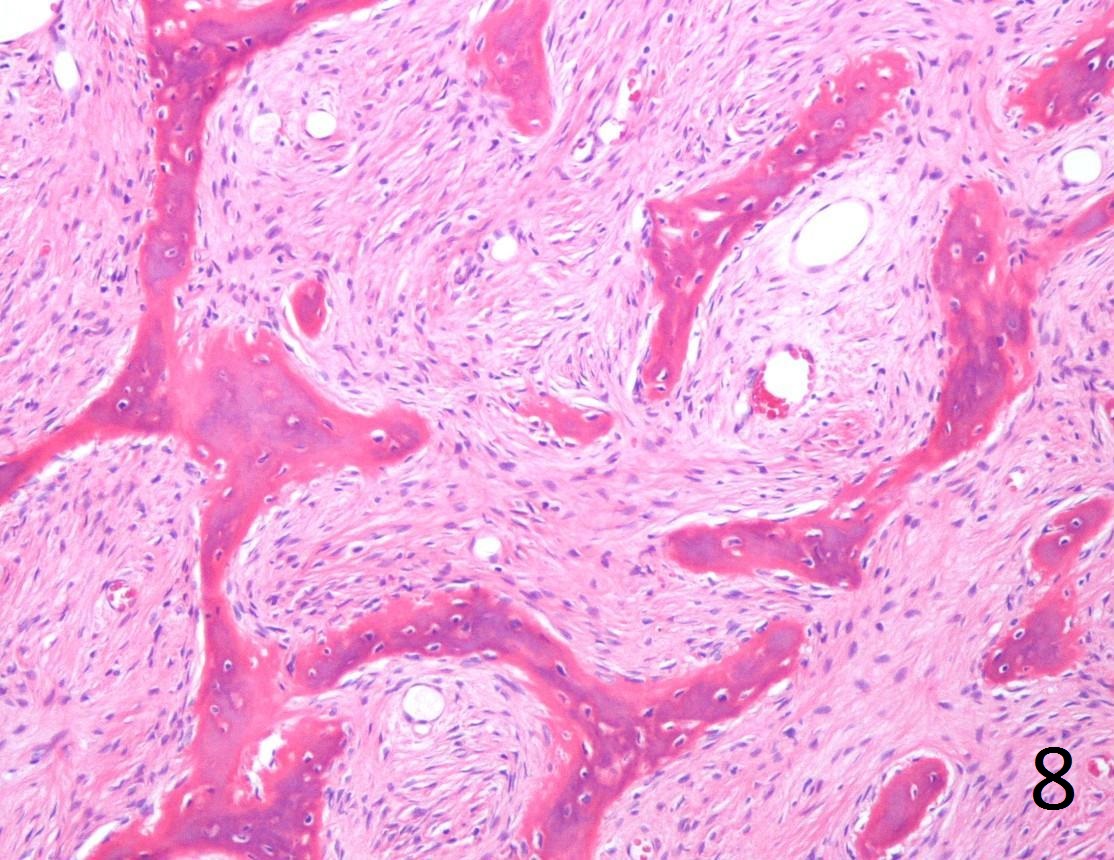 Fig. 8. Microscopic: Low power photograph of fibrous dysplasia shows a combination of bland fibrous tissue with small fragments of woven bone. The lesion is hypocellular with small uniform fibroblasts. There are spicules of bone that are not lined by osteoblasts.
Fig. 8. Microscopic: Low power photograph of fibrous dysplasia shows a combination of bland fibrous tissue with small fragments of woven bone. The lesion is hypocellular with small uniform fibroblasts. There are spicules of bone that are not lined by osteoblasts.
 Fig. 9. High power photograph of pathology of fibrous dysplasia shows woven bone being produced by the fibrous tissue. There are no osteoblasts lining the bone.
Fig. 9. High power photograph of pathology of fibrous dysplasia shows woven bone being produced by the fibrous tissue. There are no osteoblasts lining the bone.
PROGNOSIS
Biological Behavior
• Benign tumor
• Monostotic lesions have good prognosis
• Polyostotic lesions tend to be more active or aggresive
• Recurrence following curettage is common particularly when bone grafting the defect with autologous bone (one’s own bone). Cadaver bone tends to heal more reliably.
• Poor outcome is frequent in young patients with polyostotic lesions because of severe deformities and fractures
• Low chance of malignant transformation (mostly polyostotic lesions)
TREATMENT
• Can vary from observation to surgery and/or medical treatment (Bisphosphonates)
• Asymptomatic lesions can be observed
• Surgical treatment when patient complains of progressive deformity, large lesion with pain, nonunion, suspicion of malignancy, impending pathological fracture or lesions at high risk of fracturing such as those in the femoral neck and subtrochanteric region of the femur.
• Surgery usually consists of curettage and bone grafting with possible internal fixation
• Medical alternative in cases than cannot be managed surgically (Biphosphonates)
• Results with bisphosphonates are mixed
