General Information
An aneurysmal bone cyst (ABC) is a benign bone tumor or neoplasm. It consists of a blood-filled multiloculated cavity with a thick fibrous lining. The lining is composed of mesenchymal spindle cells, capillaries, multinucleated giant cells, and often, immature reactive bone formation. Aneurysmal bone cyst was first described in 1942 by Jaffe and Lichtenstein.
Clinical Data
• Rare; 0.14 to 0.32 per 100,000
• Most common in first two decades
• Equal frequency in males and females
• Most Common tumor of pelvis in pediatric population
• Second most common tumor of spine.
The distal femur and proximal tibia are the most common sites of involvement although ABCs have been reported in virtually every bone.
The lesion usually involves the medullary canal but can arise within the cortex or subperiosteal.
Most arise in the metaphysis of the bone.
Differential diagnosis
• Unicameral bone cyst
• Chondromyxoid Fibroma
• Giant cell tumor
• Telangiectatic osteosarcoma
• Secondary aneurysmal bone cyst (An ABC that arises from a different pre-existing tumor such as a giant cell tumor)
Clinical Presentation
Signs/symptoms
• Mild to moderate pain
• Swelling
• Palpable expansile mass
Prevalence
Male > Female 1.3:1
Age
Most cases occur between 10 to 30 years of age.
It is most commonly found during the second decade of life.
It is one of the most common bone tumors in children.
Sites
• Femur 52%
• Tibia 52%
• Humerus 52%
• Fibula 52%
• Skull
• Spinal Column (posterior column)
Metaphyseal regions of bones.
Radiographic Presentation
• Variable sizes
• Multiple internal trabeculations
• Rapid growth
• Cortical scalloping, bone contour often expanded.
Plain x-ray
• Radiolucent
• Geographic and Eccentric lesion that is well circumscribed
• May scallop or expand the surrounding cortex
• Surrounded by sclerotic bone
• Methaphyseal region most common
• Eccentric
• Elevation of the periosteum could be seen as a benign appearing periosteal reaction (continuous periosteal reaction)

Fig 1a. Plain X-ray (AP View). ABC of the Distal Tibia: Geographic Well Circumscribed Lesion in the distal tibia. The cortices are expanded. There are internal septations. There is no internal mineralization. There is no evidence of a malignant appearing periosteal reaction such as a sunburst or hair on end pattern or codman’s triangle.

Fig 1b: Plain X-ray (Lateral View): ABC of Distal Tibia. Notice how the cortices or bony contour appears expanded. The tumor has been eroding the inner aspect of the cortex of the bone. In response the periosteum on the outside lays down new bone which gives the bone and expanded contour.
MRI
- Geographic well circumscribed
- High signal on T2 weighted MRI images
- Fluid/Fluid level (T2) are highly characteristic
Fig 2 a-e. MRI of an ABC of Distal Tibia: Fig 2 a-c: geographic cystic expansile lesion with fluid-fluid levels. The fluid-fluid levels are caused by bleeding into the cavities. The blood collects and the degredation products settle to the gravity dependent areas of the cavities. This shows up as fluid-fluid levels on the MRI. Fig 2 d,e: This is a gadolinium enhanced MRI of the ABC of the distal tibia. There is peripheral and septal enhancement indication cyst formation. The contrast outlines the cystic cavities but does not enter into the center
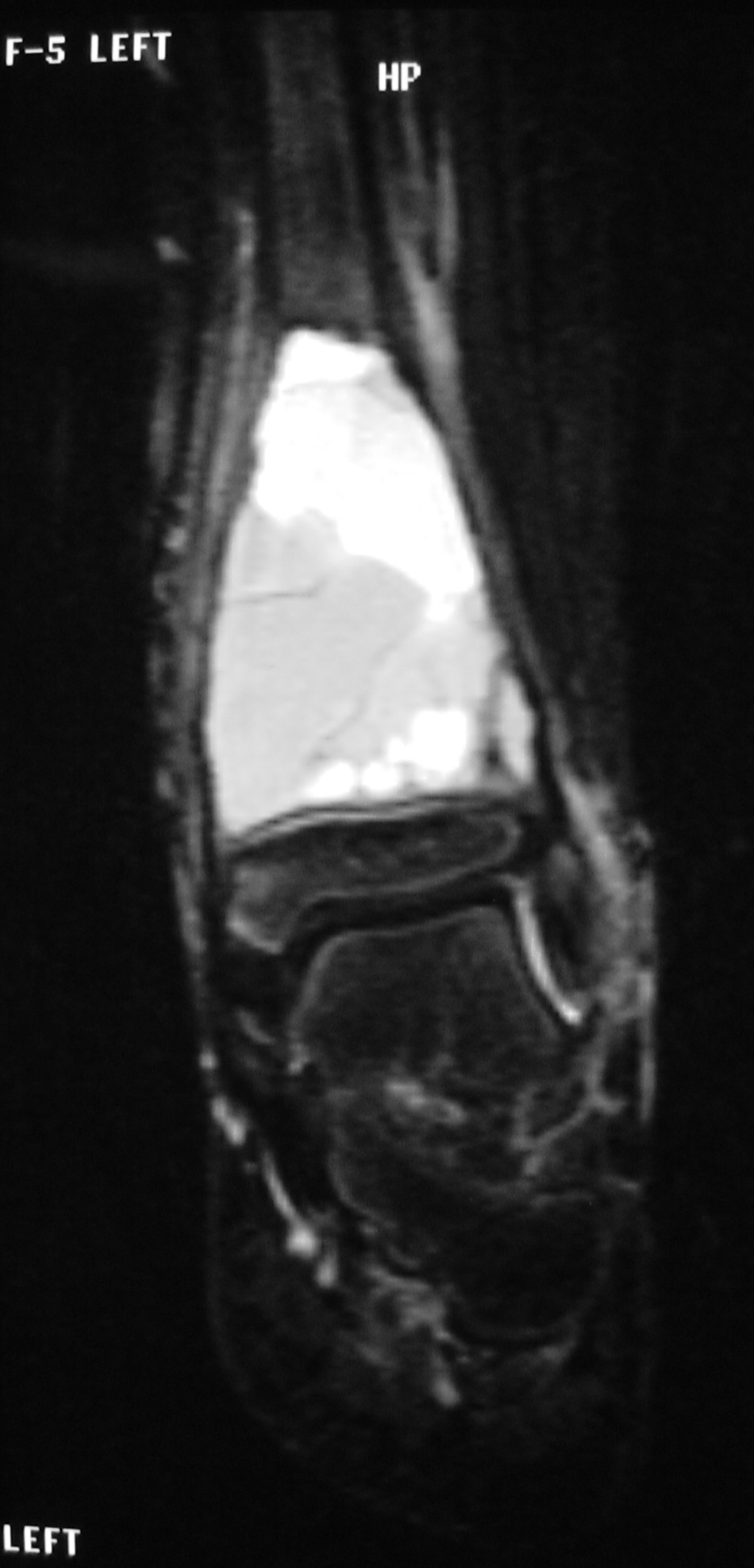
Fig 2 a: Coronal T2 weighted MRI of an ABC
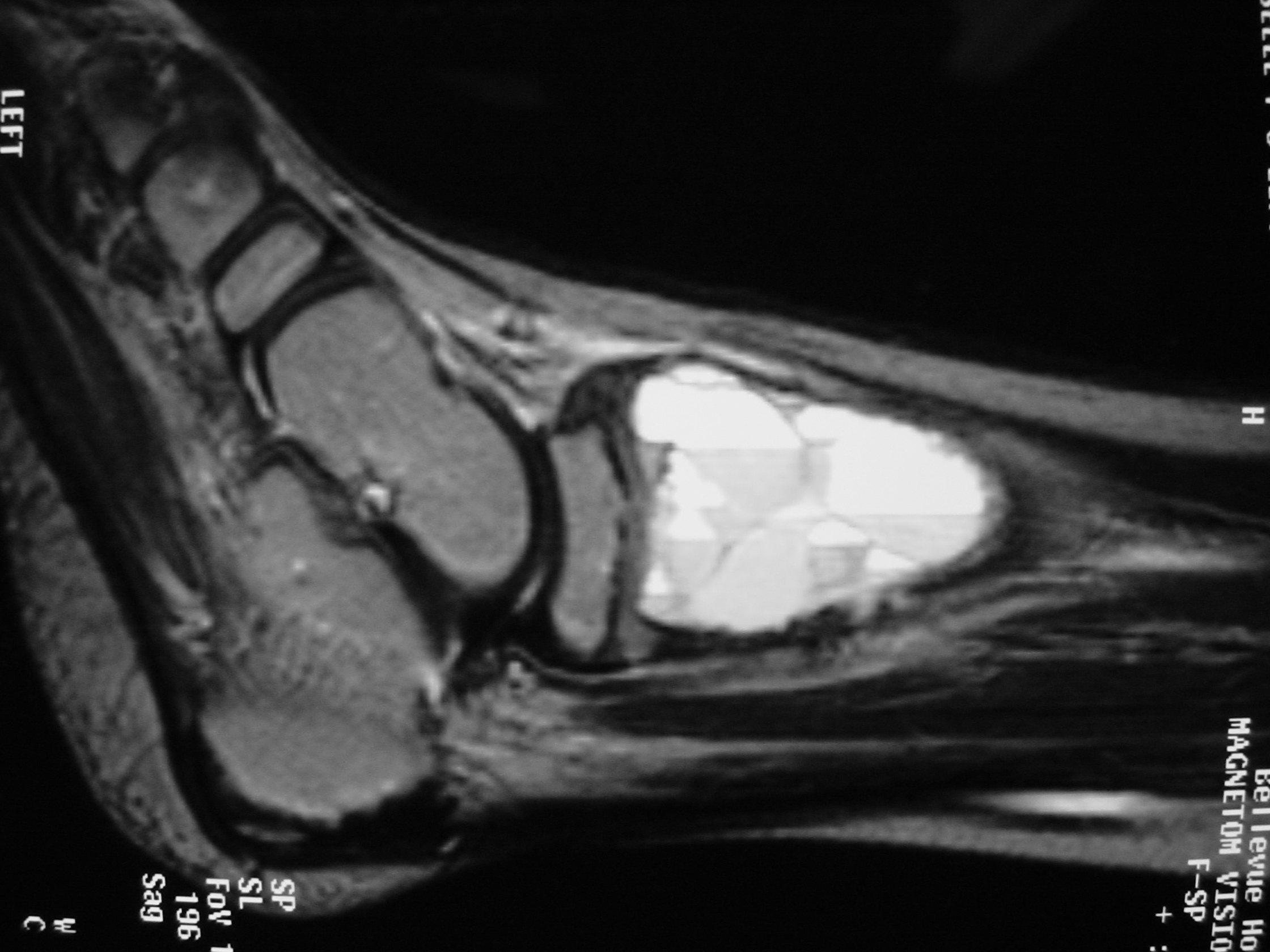
Fig 2b: Sagittal T2 weighted MRI of and ABC
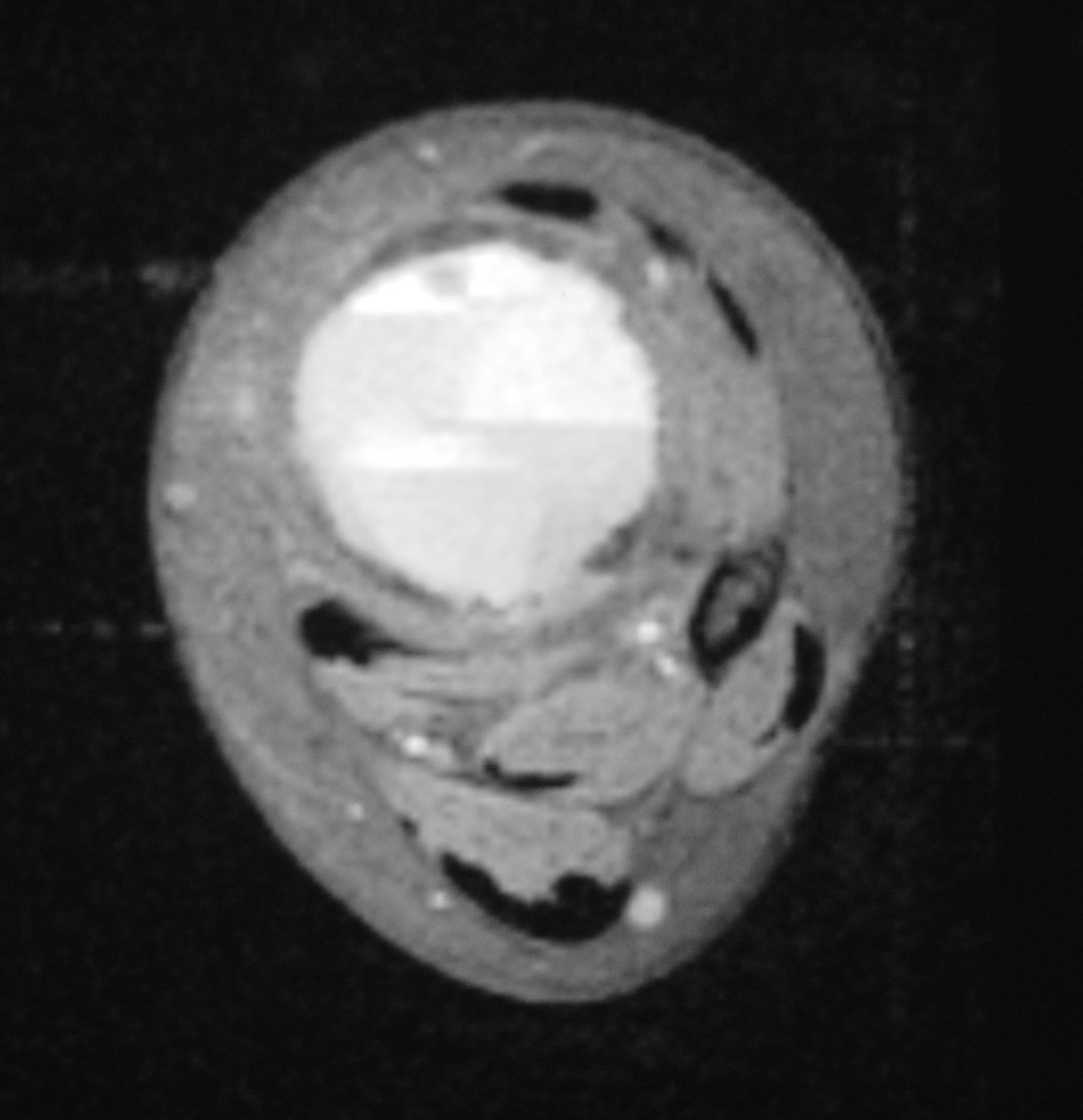
Fig 2c: Axial T2 weighted MRI of an ABC
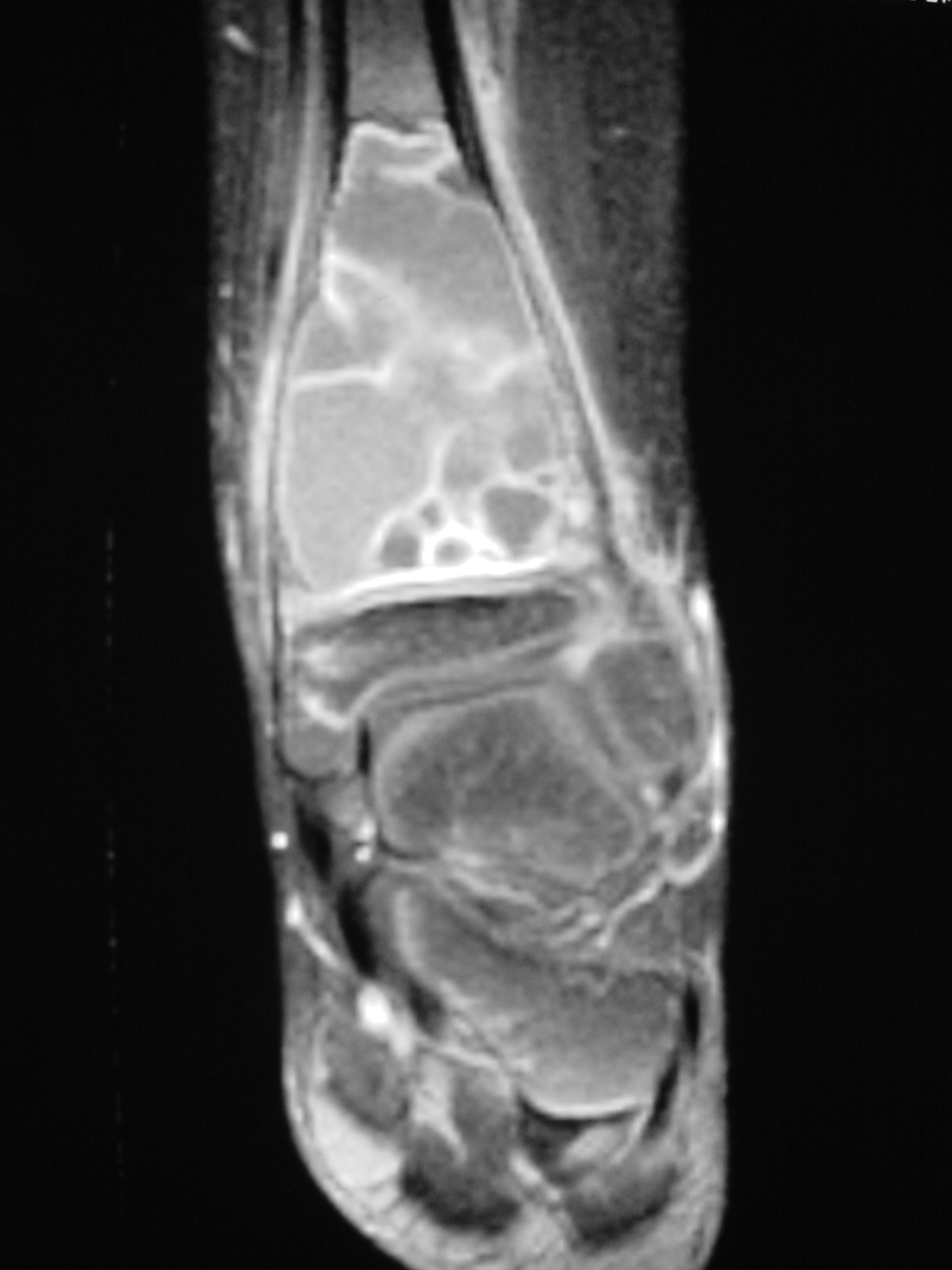
Fig 2d: Coronal gadolinium enhanced MRI of an ABC
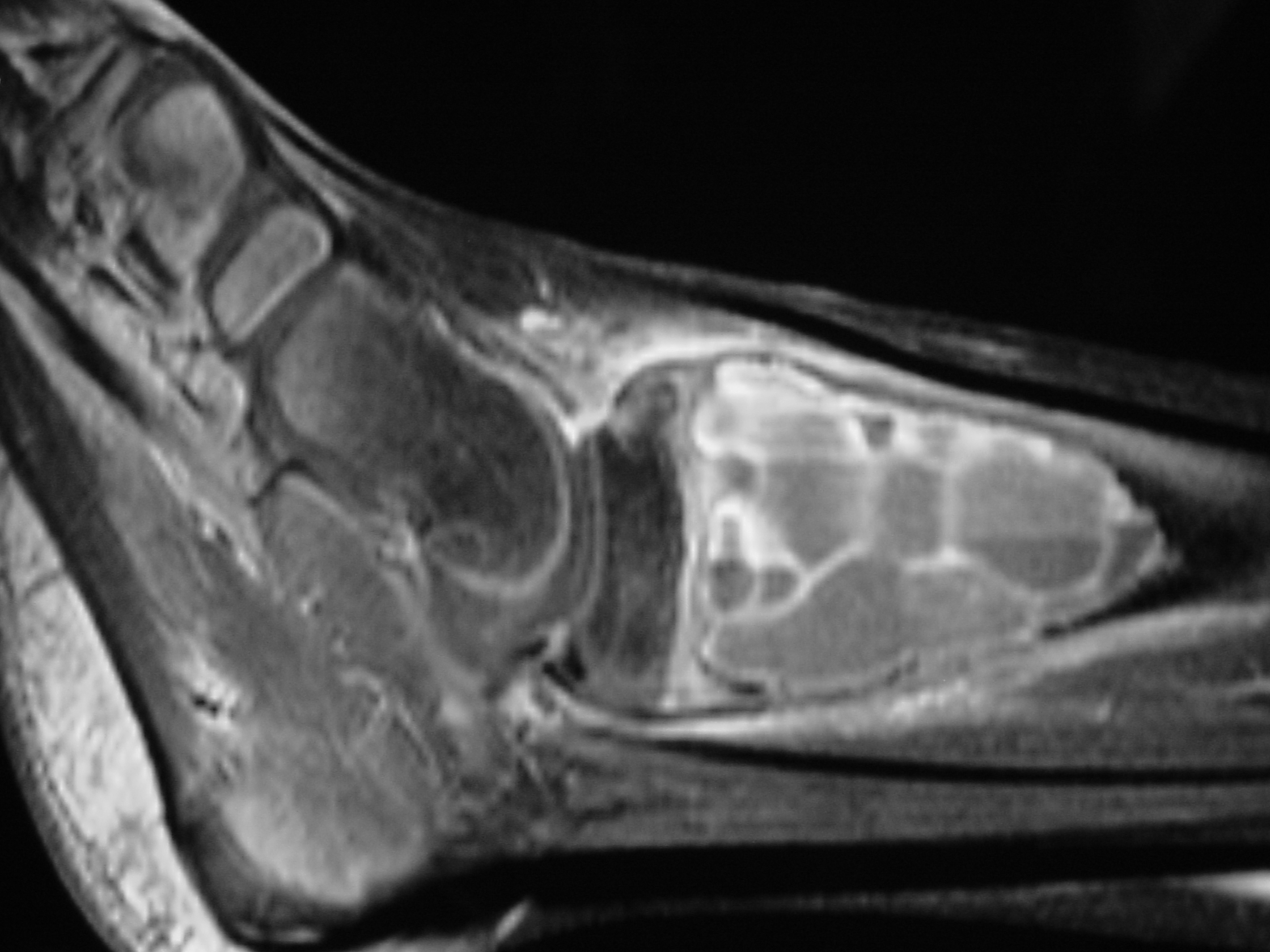
Fig 2e: Sagittal gadolinium enhanced MRI of an ABC
Gross Pathology
- Hemorrhagic tissue with cystic cavities
- No clots with solid aggregates of tissue
- Eggshell”-thin layer of periosteal new bone.
Microscopic Pathology
- Hemorrhagic tissue with large cavitary spaces divided by septum of spindle fibroblastic cells, inflammatory cells and few giant cells.
- Osteoid formation could be noted (reactive and benign in nature)
Fig 3 a,b,c. Microscopic pathology of an Aneurysmal Bone Cyst (ABC):
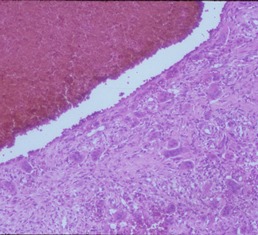
Figure 3a: There is a large blood filled cystic cavity surrounded by a fibrous septae that includes benign appearing spindle cells, fibrous extracellular matrix and scattered giant cells. There are areas of reactive bone formation. The fibroblastic cells are bland appearing. There are no abnormal mitotic figures.
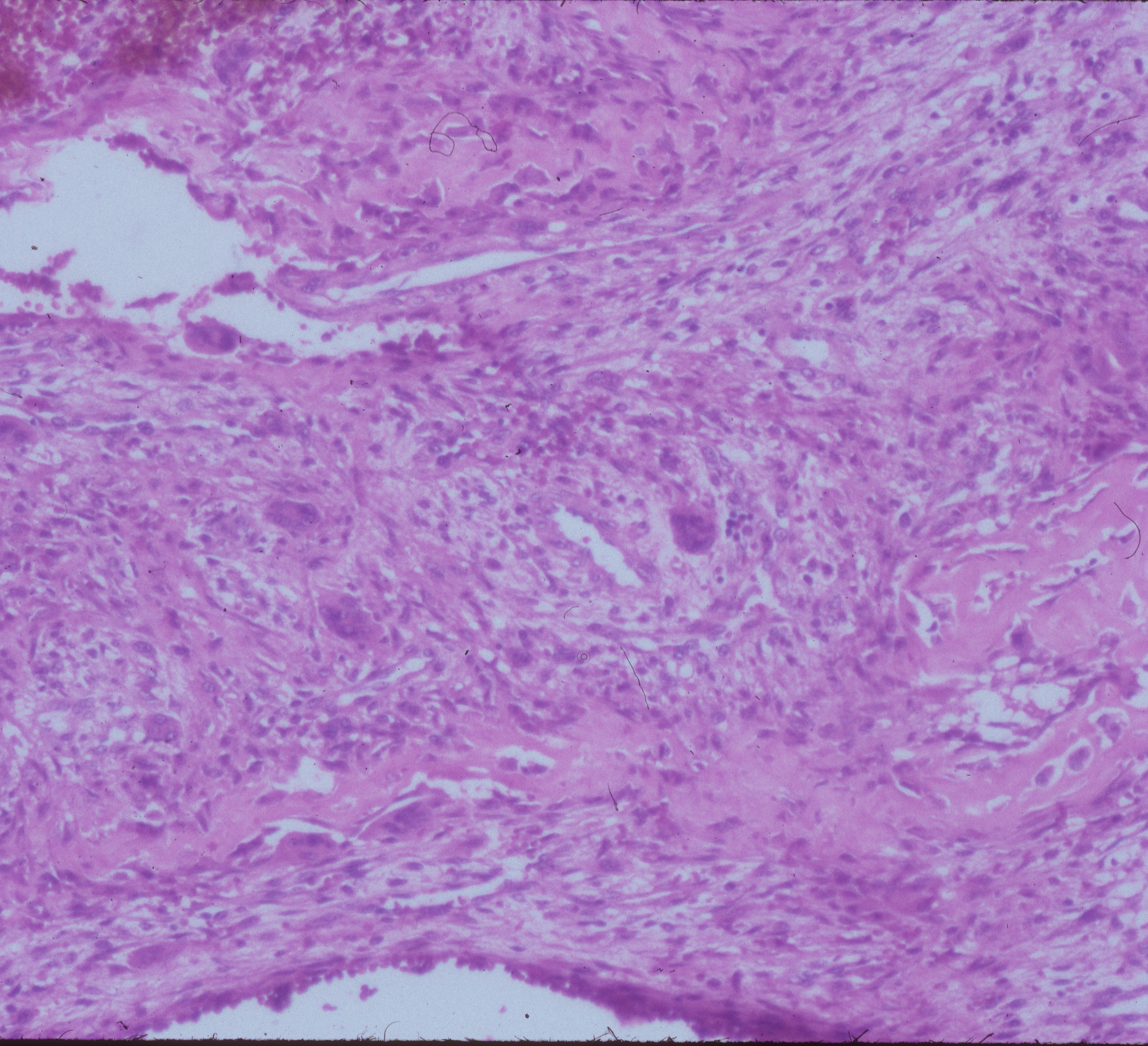
Fig 3b: Intermediate power of a septum of an ABC: There is no epithelial lining around the wall of the cavity filled with blood. There are spindle cells and scattered giant cells.
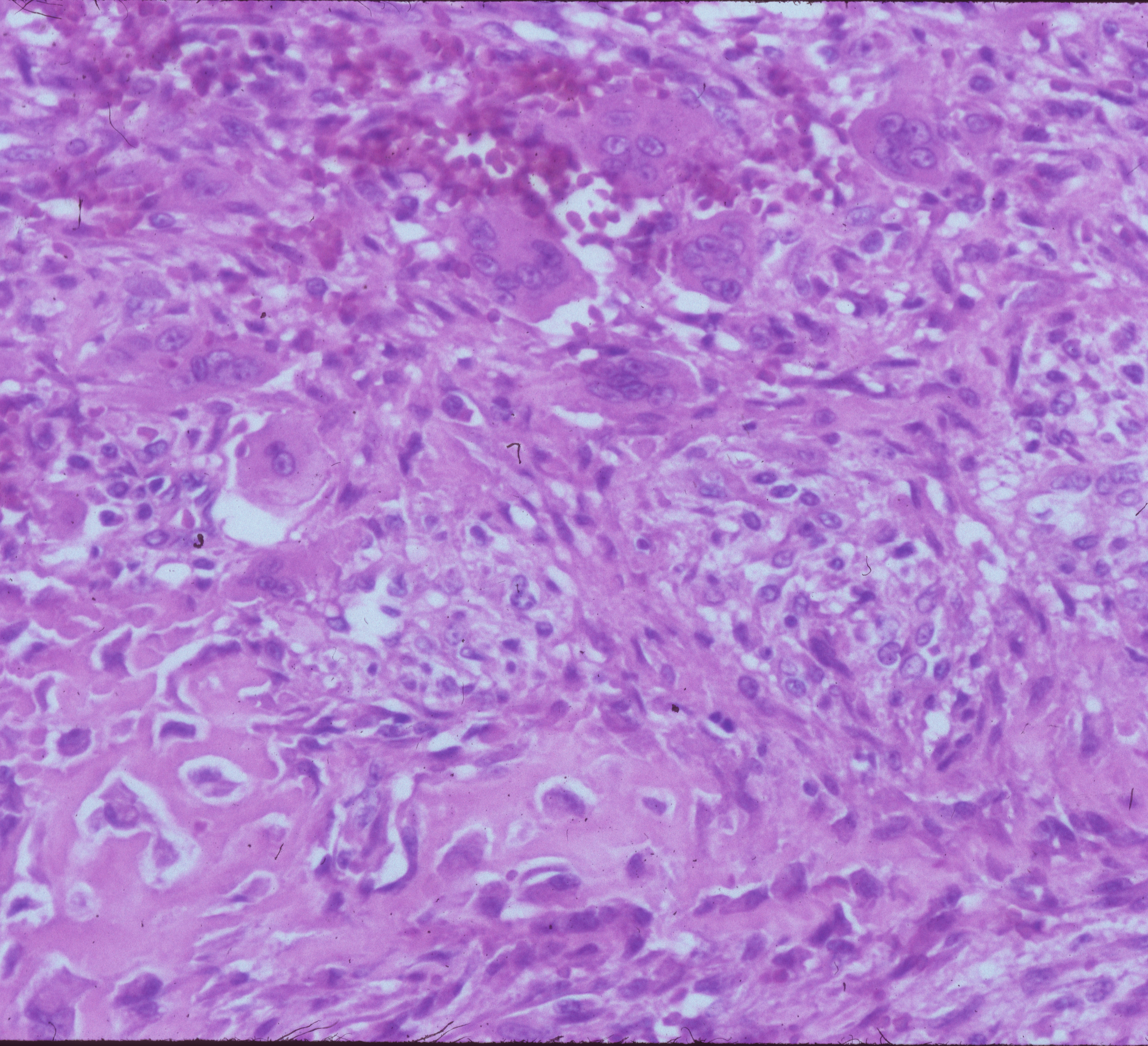
Fig 3c: High power view of an ABC: Demonstrates reactive bone formation within the wall of the cystic cavities. This is reactive bone and different from the lace like immature bone layed down by an osteosarcoma
- ABCs are benign aggressive tumors that destroy bone
- Normally ABCs never invade the surrounding soft tissue
- Could be associated with other tumors like Giant Cell Tumor, Osteoblastoma and Chondroblastoma. These are called secondary ABCs because they arise from a preexisting tumor.
- There is at least a 20% risk of recurrence after curettage, depending on location and the proportion of cellular tissue, amount of osteoid and fibroblastic component.
o Mitotic index > 7 per 50 fields associated with higher recurrence rate.
- Rarely, ABCs can transform into a malignant tumor. In the past, this has generally been associated with radiation treatments treatments. Radiation is typically not used in the treatment of this tumor any longr.
Treatment
- Intralesional curettage and bone grafting
- Adjuvant therapy is frequently used to eliminate microscopic tumor cells and decrease the risk of local recurrence
o Cryotherapy reduces the risk of local recurrence to an overall rate of 5%
- For large unresectable tumors an embolization can be considered in an attempt to cut off the blood supply and essentially kill the ABC
- Long term follow up is recommended to evaluate for recurrence.
- Rarely irradiation is used for the rare lesion that acts especially aggressive however there is a risk of cancerous transformation in the future. Dr. Wittig has never encountered an ABC that required treatment with radiation or embolization
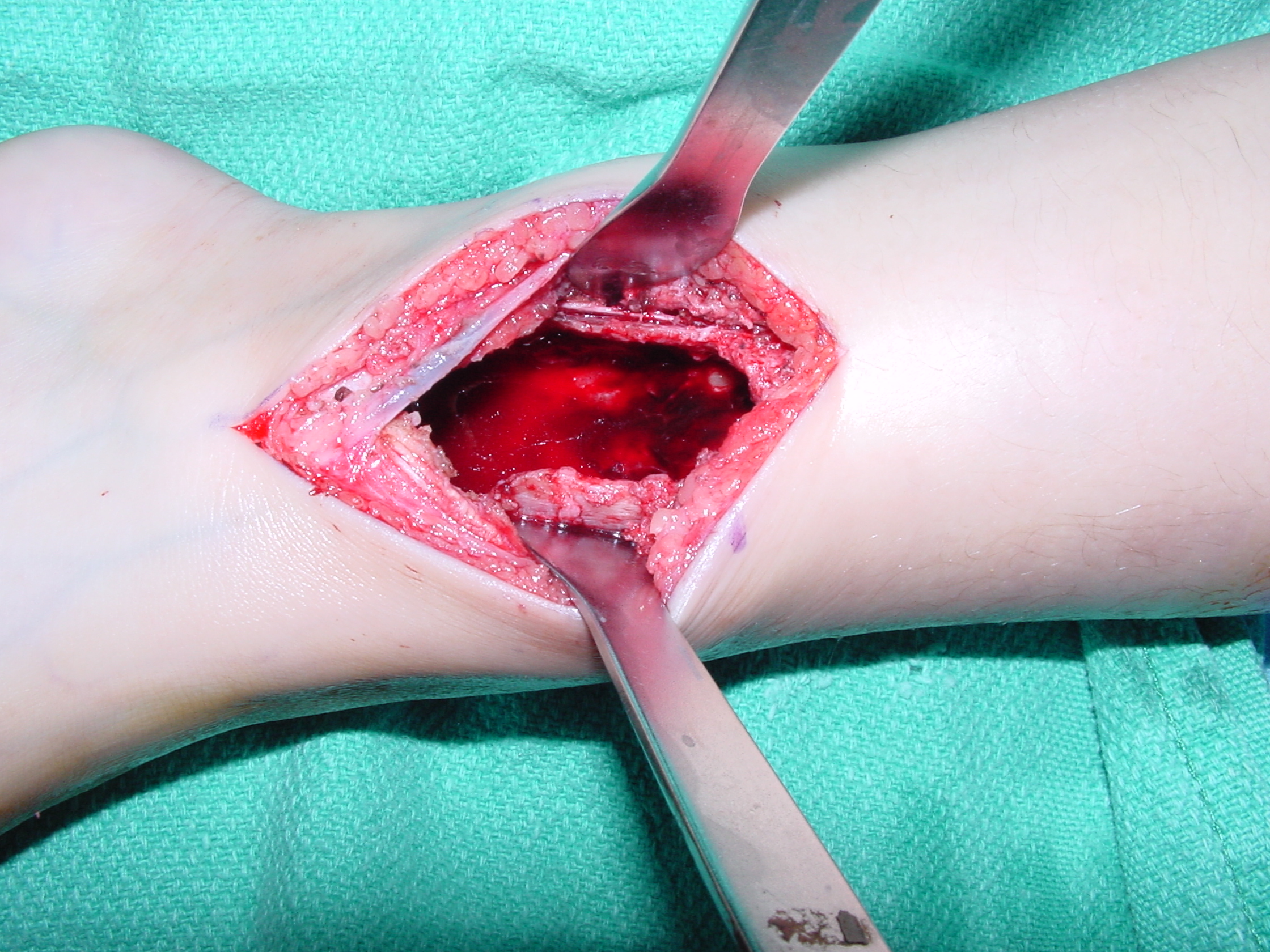
Fig 4. Intraoperative photograph showing a curettage of an ABC of the distal tibia through a medial approach. The tumor is usually curetted and then the cavity is shaved down with a midas rex burr. This is called a resectional curettage and reduces the risk of local recurrence. Additional adjuvants such as liquid nitrogen may be used to treat the cavity and irradicate microscopic tumor cells. The cavity is usually filled with bone graft or bone cement. Fixation devices may be used in specific situations to prevent postoperative fracture.
